 Provider News KentuckyJanuary 1, 2025 January 2025 Provider Newsletter Featured Articles Quality Management | Commercial / Medicare Advantage / Medicaid | November 7, 2024 Education & Training | Commercial / Medicare Advantage | January 1, 2025 Products & Programs | Commercial | January 1, 2025
KYBCBS-CRCM-074622-24 HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). On January 1, 2025, we launched Health Perks, a new incentive program that rewards members for completing select healthcare activities. This program is available for a select number of our plans. Please confirm member eligibility before promoting the program benefits. For more information or to verify eligibility, benefits, or account details, call the number located on the back of the member’s ID card. Limited health plan eligibilityThese are the Health Perks plans eligible for rewards. Plan number | State | Plan | H4346-014-000 | CO | Anthem Dual Advantage (HMO D-SNP) | H2836-006-000 | CT | Anthem Full Dual Advantage (PPO D-SNP) | H5854-008-000 | CT | Anthem Full Dual Advantage 2 (HMO D-SNP) | H5854-013-000 | CT | Anthem Full Dual Advantage Select (HMO D-SNP) | H4036-032-000 | GA | Anthem Full Dual Advantage (PPO D-SNP) | H4036-039-000 | GA | Anthem Dual Advantage (PPO D-SNP) | H5422-018-000 | GA | Anthem Dual Advantage (HMO D-SNP) | H5422-019-000 | GA | Anthem Full Dual Advantage (HMO D-SNP) | H3447-020-000 | IN | Anthem Full Dual Advantage (HMO D-SNP) | H3447-046-000 | IN | Anthem Dual Advantage (HMO D-SNP) | H3447-048-000 | IN | Anthem Full Dual Advantage Aligned (HMO D-SNP) | H3447-055-000 | IN | Anthem Full Dual Advantage Aligned NFLOC (HMO D-SNP) | H9525-007-000 | KY | Anthem Full Dual Advantage (HMO D-SNP) | H9525-016-000 | KY | Anthem Dual Advantage (HMO D-SNP) | H9525-019-000 | KY | Anthem Full Dual Advantage 2 (HMO D-SNP) | H3447-018-000 | MO | Anthem Full Dual Advantage (HMO D-SNP) | H3447-047-000 | MO | Anthem Dual Advantage (HMO D-SNP) | H3447-053-000 | MO | Anthem Full Dual Advantage 2 (HMO D-SNP) | H4346-025-000 | NV | Anthem Full Dual Advantage (HMO D-SNP) | H4346-026-000 | NV | Anthem I Carelon Full Dual Advantage (HMO D-SNP) | H8432-041-000 | NY | Anthem HealthPlus Full Dual Advantage LTSS (HMO D-SNP) | H8432-042-000 | NY | Anthem HealthPlus Full Dual Advantage (HMO D-SNP) | H3655-033-000 | OH | Anthem Full Dual Advantage (HMO D-SNP) | H3655-048-000 | OH | Anthem Dual Advantage (HMO D-SNP) | H3655-049-000 | OH | Anthem Full Dual Advantage 2 (HMO D-SNP) | H2441-001-000 | VA | Wellpoint Dual Advantage 2 (HMO D-SNP) | H9525-003-000 | WI | Anthem Full Dual Advantage (HMO D-SNP) | H9525-012-000 | WI | Anthem Dual Advantage (HMO D-SNP) | H9525-018-000 | WI | Anthem Full Dual Advantage 2 (HMO D-SNP) |
Health Perks rewardsThese are the eligible healthcare activities, member rewards, and claim codes. Healthcare activity | Reward amount | Eligible claim codes | Annual wellness visit/annual physical | $30 | 99381, 99382, 99383, 99384, 99385, 99386, 99387, 99391, 99392, 99393, 99394, 99395, 99396, 99397, 99401, 99402, 99403, 99404, 99411, 99412, G0438, G0439, G0463, G0468, Z00.00, Z00.01, Z00.8 | Breast cancer screening | $20 | 77061, 77062, 77063, 77065, 77066, 77067 | Colorectal screening | $30 | 4522, 4523, 4525, 4542, 4543, 44388, 44389, 44390, 44391, 44392, 44394, 44401, 44402, 44403, 44404, 44405, 44406, 44407, 44408, 45378, 45379, 45380, 45381, 45382, 45384, 45385, 45386, 45388, 45389, 45390, 45391, 45392, 45393, 45398, G0105, G0121, 74261, 74262, 74263, 4524, 45330, 45331, 45332, 45333, 45334, 45335, 45337, 45338, 45340, 45341, 45342, 45346, 45347, 45349, 45350, G0104 | Fecal occult blood test | $10 | 82270, 82274, G0328, 81528 | Bone density screening | $10 | 8898, 76977, 77078, 77080, 77081, 77085, 77086, BP48ZZ1, BP49ZZ1, BP4GZZ1, BP4HZZ1, BP4LZZ1, BP4MZZ1, BP4NZZ1, BP4PZZ1, BQ00ZZ1, BQ01ZZ1, BQ03ZZ1, BQ04ZZ1, BR00ZZ1, BR07ZZ1, BR09ZZ1, BR0GZZ1, J0897, J1740, J3489, J3110, J3111 | Flu vaccine | $10 | 90630, 90653, 90654, 90656, 90658, 90661, 90662, 90673, 90674, 90682, 90686, 90688, 90689, 90694, 90756, 90660, 90672 |
Claim coverage notes:- For colonoscopies, annual wellness visits, and breast cancer screenings, members will not have out‑of‑pocket costs or a copayment when performed by an in‑network provider:
- Note: A cost share may be applicable for any additional services or tests conducted during the visit for each service listed in the healthcare activity chart above.
- For bone density screenings, Medicare Part B (for doctor visits, outpatient procedures, preventive services, home health services, and DME) covers this test once every 24 months (or more often if medically necessary) when at least one of the following conditions is met:
- Their care provider has determined they are estrogen‑deficient and at risk for osteoporosis based on their medical history and other findings.
- Their X‑rays show possible osteoporosis, osteopenia, or vertebral fractures.
- They are taking prednisone or steroid‑type drugs or are planning to begin this treatment.
- They have been diagnosed with primary hyperparathyroidism.
- They are being monitored to see if their osteoporosis drug therapy is working.
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-075375-24-CPN75369, MULTI-BCBS-CR-078045-25 At a glance: - The Consolidated Appropriations Act (CAA) requires care providers to validate their online directory details every 90 days to remain listed.
- Anthem's provider data management (PDM) on Availity Essentials enables care providers to verify and update their information efficiently.
- Care providers can submit data updates through the PDM's Roster Automation solution using a standard Microsoft Excel document.
The CAA of 2021 requires care providers to review and verify the accuracy of the following information in the online provider directory every 90 days: - Provider/facility name
- Address
- Specialty
- Phone number
- Digital contact information
Providers who fail to verify their information every 90 days may be removed from the online provider directory. Providers will be reinstated to the online provider directory once verification is complete. Anthem uses a proactive monitoring and correction program to further ensure provider directory data is accurate. The program uses technology and various data sources to confirm the status and accuracy of the directory data. Providers may be removed from the directory when it is determined the provider data is inaccurate. Review, verify, and update your directory informationTo review, verify, and update your online directory information, Anthem uses the provider data management (PDM) capabilities of Availity Essentials to update provider or facility data. Using the Availity PDM application meets the verification requirement to validate provider demographic data set by the CAA. PDM features include: - Updating provider demographic information for all assigned payers in one location.
- Verifying and managing current provider demographic information.
- Monitoring submitted demographic updates in real-time with a digital dashboard.
- Reviewing the history of previously verified data.
To access the PDM application, log on to https://Availity.com and go to My Providers > Provider Data Management. Administrators are automatically granted access to PDM. Additional staff may be given access to PDM by an administrator. To find your administrator, go to My Account Dashboard > My Account > Organization(s) > Administrator Information. View the Availity PDM quick start guide here (PDF). Use Roster Automation to submit provider demographic changesWithin the PDM application, providers also have the choice and flexibility to request data updates using our Roster Automation solution by submitting a spreadsheet via a roster upload. Provider data additions, changes, and terminations, including requests to suppress a provider from provider directories, are submitted on a standardized Microsoft Excel document. Provider suppression should occur for office locations at which the provider does not routinely accept patient appointments (for example, the provider only covers/floats at that location). The resources for this process are available on our website. Visit Anthem.com > For Providers > Forms and Guides. The following two resources appear under the Digital Tools category: - Roster Automation Rules of Engagement: This is a reference document available to ensure error-free submissions for accurate and timely updates through automation.
- Roster Automation Standard Template: Use this template to submit your information. More detailed instructions on formatting and submission requirements can be found on the first tab of the template, User Reference Guide.
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CM-072651-24-CPN72642 At a glance:
- Total Member View (TMV) provides a full 360‑degree view of patient health and treatment history.
- Easily identify and provide feedback on patients missing essential preventive screenings, follow‑up appointments, or necessary treatments.
- User‑friendly guides available for seamless navigation and usage of TMV.
TMV is a dashboard you can access through Payer Spaces in the Availity Essentials platform that gives you a full 360‑degree view of your patient’s health and treatment history to help you facilitate care coordination. You can drill down to specific items in a patient’s medical record to retrieve demographic information, care summaries, claims details, authorization details, pharmacy information, and care management‑related activities.
TMV is replacing the previous Patient 360 (P360) dashboard that you may have used to access your patient’s medical records. The TMV user interface is purple and says Total Member View in the upper right corner. TMV highlights include viewing your patients who have a care gap and providing feedback on care gaps. If you were a user of the P360 dashboard, moving to Total Member View will be a simple transition.
Viewing your patients who have a care gap:
- After selecting the Total Member View application tile in Payer Spaces, you will be taken to the Summary tab.
- Within the Summary tab, locate and select the care gap alert name on the Active Alerts card.
Providing feedback on care gaps:
- Select the line item of the care gap on the Active Alerts card you would like to provide feedback on. A Care Gap Alert Feedback Entry dialog box will display.
- From the Latest Feedback field, select the drop‑down arrow, then select the type of feedback you would like to provide (for example, My Patient is compliant with message suggestion, My Patient will not likely comply with this suggestion).
- Once selected, choose Save.
User guide
The Total Member View Availity User Guide illustrates step‑by-step instructions on accessing and navigating through the Availity Essentials platform and how to use the system. This guide is available through the Digital Solutions Learning Hub.
We are committed to finding solutions that help our care provider partners offer quality services to our members. Anthem Blue Cross and Blue Shield Medicaid is the trade name of Anthem Kentucky Managed Care Plan, Inc. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. KYBCBS-CDCRCM-071432-24 At a glance: - Care providers will use the Error Report function in Availity Essentials to identify, rectify, and resubmit errors in rosters.
- The new Results Report is available to view.
- Both the Error and Results Reports can be found on the Upload Roster File page of Availity, with additional guidance available in the Roster Submission Guide.
Error Report an essential tool to identify and correct mistakesAs previously communicated in November, we introduced an Error Report to the Upload Roster File screen in Availity Essentials Provider Data Management (PDM). Care providers can use this Error Report to understand where errors occurred (specifically which sheet, tab, and row), the cause of the issue, and how to fix it. As a reminder, you will need to correct any errors submitted in a roster (for example, missing data or incorrectly formatted data) in the future. Rows in a roster that contain an error will not be processed and the addition, change, or termination will not be updated in our systems. Effective November 15, 2024, care providers are responsible for using the Error Report to identify errors in a roster, correct them, and resubmit the roster rows that contain errors. Rows in a roster that contain an error will not be processed and the addition, change, or termination will not be updated in our systems. New Results Report identifies added and updated recordsFor better transparency for our care providers, we’ve now introduced a new Results Report that allows care providers to see the number of unique records that were added or updated based on a specific roster. The Results Report also contains data elements associated with the records, including NPI, TIN, name, address, and effective date. Think of it as a receipt of the actions taken to keep your demographic information accurate. A Results Report has been created for rosters received on and after June 15, 2024. Both reports are on the Upload Roster File page of Availity You can find the Results Report, as well as the Error Report, on the Upload Roster File page of Availity PDM. Future informational webinars are coming soon — Watch for updates in the Provider Newsletter. Use the Roster Submission Guide Additional information about the Results Report and Error Report can be found in our Roster Submission Guide. Find it online at https://Availity.com > Payer Spaces > Select Payer Tile > Resources > Roster Submission Guide using Provider Data Management. We look forward to working together to achieve improved outcomes. Anthem Blue Cross and Blue Shield Medicaid is the trade name of Anthem Kentucky Managed Care Plan, Inc. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. KYBCBS-CDCRCM-072280-24-CPN71750 We’re excited to introduce two new Payment Integrity trainings available on our Digital Solutions Learning Hub: - Payment Integrity: Emergency Dept Evaluation and Management Services
- Payment Integrity: Outpatient Evaluation and Management Services
With an initial focus on these two key educational initiatives, our purpose is to amplify your billing and coding accuracy. More trainings will be announced throughout the year. Discover what our Digital Solutions Learning Hub has to offer. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc., an independent licensee of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. KYBCBS-CRCM-072244-24-CPN72085, MULTI-BCBS-CRCM-072264-24-CPN72085, MULTI-BCBS-CRCM-075953-24-CPN75258, MULTI-BCBS-CRCM-077839-25-CPN77515, MULTI-BCBS-CRCM-080188-25-CPN79720 We’re excited to introduce two new Payment Integrity trainings available on our Digital Solutions Learning Hub: Payment Integrity: Emergency Dept Evaluation and Management Services and Payment Integrity: Outpatient Evaluation and Management Services. With an initial focus on these two key educational initiatives, our purpose is to amplify your billing and coding accuracy. More trainings will be announced throughout the year. Discover what our Digital Solutions Learning Hub has to offer. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc., an independent licensee of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. KYBCBS-CRCM-072244-24-CPN72085 Effective January 9, 2025 Summary: On September 20, 2024 and October 2, 2024 the Pharmacy and Therapeutic (P&T) Committee approved the following Clinical Criteria applicable to the medical drug benefit for Anthem. These policies were developed, revised, or reviewed to support clinical coding edits. Visit Clinical Criteria to search for specific policies. For questions or additional information, use this email. Please see the explanation/definition for each category of Clinical Criteria below: - New: newly published criteria
- Revised: addition or removal of medical necessity requirements, new document number
- Updates marked with an asterisk (*) notate that the criteria may be perceived as more restrictive
Please share this notice with other members of your practice and office staff. Please note: - The Clinical Criteria listed below applies only to the medical drug benefits contained within the member’s medical policy. This does not apply to pharmacy services.
- This notice is meant to inform the provider of new or revised criteria that has been adopted by Anthem only. It does not include details regarding any authorization requirements. Authorization rules are communicated via a separate notice.
Effective date | Clinical Criteria number | Clinical Criteria title | New or revised | January 9, 2025 | *CC-0267 | Ebglyss (lebrikizumab-lbkz) | New | January 9, 2025 | *CC-0268 | Lymphir (denileukin diftitox-cxdl) | New | January 9, 2025 | *CC-0269 | Nemluvio (nemolizumab-ilto) | New | January 9, 2025 | *CC-0270 | Niktimvo (axatilmab-csfr) | New | January 9, 2025 | *CC-0271 | Tecelra (afamitresgene autoleucel) | New | January 9, 2025 | *CC-0012 | Brineura (cerliponase alfa) | Revised | January 9, 2025 | *CC-0250 | Veopoz (pozelimab-bbfg) | Revised | January 9, 2025 | *CC-0072 | Vascular Endothelial Growth Factor (VEGF) Inhibitors | Revised | January 9, 2025 | *CC-0029 | Dupixent (dupilumab) | Revised | January 9, 2025 | CC-0201 | Rybrevant (amivantamab-ymjw) | Revised | January 9, 2025 | CC-0130 | Imfinzi (durvalumab) | Revised | January 9, 2025 | *CC-0002 | Colony Stimulating Factor Agents | Revised | January 9, 2025 | CC-0050 | Monoclonal Antibodies to Interleukin-23 | Revised | January 9, 2025 | *CC-0011 | Ocrevus (ocrelizumab)/Ocrevus Zunovo (ocrelizumab/hyaluronidase-ocsq) | Revised |
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-071481-24-CPN71236 Effective for dates of service on and after April 23, 2025, the following updates will apply to the Carelon Medical Benefits Management Clinical Appropriateness Guidelines. As part of the Carelon Medical Benefits Management guideline annual review process, these updates focus on advancing efforts to drive clinically appropriate, safe, and affordable healthcare services. Note, several policies and guidelines were revised to provide clarification only and are not included. Some may have expanded rationales, medical necessity indications or criteria and some may involve changes to policy position statements that might result in services that previously were covered being found to be not medically necessary. Advanced Imaging/RadiologyOncologic Imaging: - National Comprehensive Cancer Network (NCCN) alignments for Cancer Screening and tumor‑specific indications, largely addressing time intervals of screening or surveillance imaging
- Added FDG‑PET allowances for Colorectal Cancer and Lung Cancer (Small Cell) accounting for nondiagnostic standard imaging
Imaging of the Abdomen and Pelvis: - Tumor or neoplasm — added requirement for initial evaluation of testicular masses with US
- Endometriosis — removed US requirement for follow‑up of patients with an established diagnosis
- Obstetric indications — specified that fetal MRI is indicated in the second or third trimester
- Diffuse liver disease — removed criteria for LiverMultiScan as an alternative to MR elastography
- Abdominal and/or pelvic pain, undifferentiated — clarified language regarding initial imaging and lab evaluation
Imaging of the Chest: - Added indication for dyspnea
Genetic TestingCarrier Screening in the Reproductive Setting: - Standard carrier screening ‑ removed CBC from the list of acceptable prior testing restrictions for hemoglobinopathy screening
- Expanded Carrier screening:
- Clarified that medical records should attest to adoption or consanguinity
- Expansive criteria to allow for multigene panels to include conditions with less than 1 in 100 carrier frequencies for individuals in a consanguineous partnership
- Removed requirement that alternate biochemical tests are not available, have provided an indeterminate result, or are less accurate than genetic testing
Genetic Testing for Inherited Conditions: - Added expansive criteria to allow confirmatory genetic testing for individuals identified to have a pathogenic or likely pathogenic germline variant in genes with established clinical utility based on results of IRB‑approved clinical research studies
- Cardiac conditions:
- Expanded genetic testing criteria for hereditary cardiomyopathy syndromes in the pediatric population
- Added new expansive medical necessity criteria for hereditary aortopathies
- Neurological conditions ‑ expanded criteria to allow SOD1 genetic testing in individuals with amyotrophic lateral sclerosis (ALS) when determined to be a candidate for FDA‑approved Qalsody (tofersen) treatment
- Thrombophilia testing:
- Removed restriction of low bleeding risk in individuals with an unprovoked VTE who are planning to stop anticoagulation
- Removed criterion (last bullet) to allow F5 and F2 genetic testing for individuals contemplating estrogen use when they have a first‑degree relative with VTE and a known hereditary thrombophilia per ASH guidance
Hereditary Cancer Testing: - Removed requirement that alternate biochemical tests are not available, have provided an indeterminate result, or are less accurate than genetic testing
- Listed specific examples of somatic test findings that, per ASCO guideline, should generate consideration of germline testing (clarification)
- Expanded criteria to allow confirmatory genetic testing for individuals identified to have a pathogenic or likely pathogenic germline variant in genes with established clinical utility based on results from direct‑to-consumer genetic testing or results from an IRB‑approved clinical research study
- Adenomatous polyp syndromes:
- Added expansive criteria to include individuals with multifocal or bilateral congenital hypertrophy of retinal pigment epithelium (CHRPE)
- Added expansive criteria to include first‑, second‑, or third‑degree relatives with known pathogenic variant or clinical findings suggestive of an inherited polyposis syndrome
- Juvenile polyposis syndrome:
- Increased testing requirement for the number of juvenile polyps in the colon from three to five (restrictive)
- Cowden syndrome:
- Expanded minor criteria to include colorectal cancer and lipomas to the list of conditions that may be present
- Lynch syndrome:
- Personal history criteria expanded to include any Lynch syndrome related cancer: colorectal, endometrial, gastric, ovarian, pancreatic, urothelial, CNS glioma, biliary tract, small intestine, sebaceous adenomas or carcinomas, keratoacanthomas, or breast carcinomas with medullary features
- Li‑Fraumeni syndrome:
- Expanded the personal history criteria to include pediatric hypodiploid acute lymphoblastic leukemia
- Restricted germline testing criteria for testing as a follow‑up to TP53 positive somatic tumor test results as per ASCO guideline
- Restricted germline testing criteria for testing of unaffected first‑, second‑, or third‑degree relatives to individuals whose affected relative meets LFS personal history criteria
- Hereditary Breast Cancer:
- Expanded BRCA1/2 testing criteria to include all women <65 with personal history of breast cancer
- All individuals who are candidates for PARP inhibitor therapy are included in scope for testing
- Clarified the statement about BRCA risk models, eliminating reference to tools that are not examples of validated risk models
- Family history criteria for testing related to having a relative with multiple primary breast cancers expanded to first‑ or second‑degree relative
- Family history criteria for testing related to having a relative with epithelial ovarian, fallopian tube, or primary peritoneal cancer expanded to include first‑, second‑, or third‑degree relatives
- Family history criteria for testing related to having a relative with breast cancer who is also an individual assigned male sex at birth expanded to include first‑, second‑, or third‑degree relatives
- Family history criteria for testing related to having a relative age <50 with breast cancer expanded to be at least one relative who is a first‑, second, or third‑degree blood relative
- Hereditary epithelial ovarian cancer:
- Clarified the statement about BRCA risk models, eliminating reference to tools that are not examples of validated risk models
- Hereditary pancreatic ductal adenocarcinoma:
- Clarified the statement about BRCA risk models, eliminating reference to tools that are not examples of validated risk models
- Multi‑gene panel testing for HBOP:
- For pancreatic carcinoma, expanded the multi‑gene panel list to include CDK4
- For breast cancer, removed the following genes from the multi‑gene panel list: ATM, BARD1, CHEK2, RAD51C, and RAD51D
- Melanoma:
- Gene list expanded to 20 genes and can include CDK4 pathogenic variants
- Nevoid basal cell carcinoma syndrome:
- Expanded threshold for the number of basal cell carcinomas from 5 in a lifetime to as low as two (multiple) if this is considered out of proportion to prior skin exposure or skin type
- Removed age restriction for Lamellar calcification of the falx cerebri (major criterion)
- Endocrine neoplasms:
- Expanded criteria to include early onset GI stromal tumors to account for evaluation for SDHB gene‑deficient GIST
- Kidney cancer:
- Expanded criteria to include individuals with a personal history of various rare kidney tumors (Birt‑Hogge-Dubé syndrome, HLRCC associated renal cell carcinoma, and more)
- Expanded criteria to include unaffected individuals with two or more first‑ or second‑degree relatives with renal cell carcinoma
- Prostate Cancer:
- For individuals with low‑risk prostate cancer, criteria expanded to include family history of breast cancer in relatives assigned female at birth and age ≤50; family history of pancreatic, gastric, brain, melanoma, intestinal (colorectal or small bowel), or endometrial cancer diagnosed at age ≤50; family history of upper tract urothelial cancer(s) in first‑ or second‑degree relatives; Ashkenazi Jewish ancestry; intraductal or cribriform histology
- For individuals with an intermediate risk of prostate cancer, criteria expanded to include family history of breast cancer in relatives assigned female at birth and age ≤50; family history of pancreatic, gastric, brain, melanoma, intestinal (colorectal or small bowel), or endometrial cancer diagnosed at age ≤50; family history of upper tract urothelial cancer(s) in first‑ or second‑degree relatives
- Removed CHEK2 or PALB2 from the multi‑panel gene list for prostate cancer
- Expanded family history criteria to first‑, second‑, or third‑degree relatives with multiple primary breast cancers
- Expanded family history criteria of prostate cancer diagnosed before age 60 to include at least one first‑ or second‑degree relative
- For individuals unaffected by prostate cancer, criteria are expanded to include 11 additional family history indicators for risk of BRCA1 or BRCA2 pathogenic variants that match the Hereditary breast cancer family history criteria
- Clarified the statement about BRCA risk models, eliminating reference to tools that are not examples of validated risk models
Radiation OncologyRadiation Therapy: - Special Treatment Procedure and Special Physics Consult: limited the scenarios where special treatment procedure and special physics consult are indicated, to more closely align with recent ASTRO guidance
- Breast cancer — reduced the minimum age at which patients with invasive disease meet criteria for accelerated partial breast irradiation (APBI)
- Head and neck cancer — removed indication for neutron therapy as this is no longer routinely used.
- Lung cancer — clarified that the maximum number of fractions for SBRT is 5 in both NSCLC and SCLC
- Oligometastatic extracranial disease — added scenario for oligoprogressive extracranial disease
- Other tumor types:
- Combined criteria for IMRT, SRS, and SBRT
- Expanded criteria for SRS and SBRT to include any radiosensitive tumor
- Prostate cancer:
- Modified number of fractions indicated, due to larger dose given in each individual fraction (no change in total dose to be given)
- Added scenario for salvage treatment after prostatectomy
- Added max fraction number for salvage RT
Hydrogel Spacers: - Expanded the use of hydrogel spacers to include them in patients receiving any form of external beam radiation therapy
Proton Beam Therapy: - Added clarifying statement that generic case control plan comparison is insufficient and that patient‑specific IMRT isodose comparison is required
As a reminder, ordering and servicing providers may submit prior authorization requests to Carelon Medical Benefits Management using the following: - Access Carelon Medical Benefit Management’s provider portal directly at providerportal.com:
- Online access is available 24/7 to process orders in real time. It is the fastest and most convenient way to request authorization.
If you have questions related to guidelines, please contact Carelon Medical Benefits Management via email at medicalbenefitsmanagement.guidelines@carelon.com. Additionally, you may access and download a copy of the current and upcoming guidelines here. Carelon Medical Benefits Management, Inc. is an independent company providing utilization management services on behalf of the health plan. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc., an independent licensee of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CRCM-070978-24-CPN70767 The following Medical Polices and Clinical Guidelines were reviewed for Indiana, Kentucky, Missouri, Ohio, and Wisconsin. To view Medical Policies and utilization management guidelines, go to anthem.com > Select Providers > Select your state > Under Provider Resources > Select Policies, Guidelines & Manuals. To help determine if prior authorization is needed for Anthem members, go to anthem.com > select Providers > select your state > under Claims > select Prior Authorization. You can also call the prior authorization phone number on the back of the member’s ID card. To view Medical Policies and utilization management guidelines applicable to members enrolled in the Blue Cross and Blue Shield Service Benefit Plan (commonly referred to as the Federal Employee Program® (FEP®)), please visit fepblue.org > Policies & Guidelines. Below are the new Medical Policies and/or Clinical Guidelines that have been approved.* Denotes prior authorization required Policy/guideline | Information | Effective date | *DME.00052 Brain Computer Interface Rehabilitation Devices | Brain computer interface rehabilitation devices, including but not limited to electroencephalography (EEG)‑driven upper extremity powered exercisers, are considered INV&NMN Existing HCPCS code E0738 effective 4/1/2024 for IpsiHand is considered INV&NMN for all indications | April 1, 2025 | *LAB.00051 Per‑ and Polyfluoroalkyl Substances PFAS Testing | Testing for PFAS substances is considered INV&NMN for all indications Existing CPT® PLA codes 0394U, 0457U for PFAS tests, and codes 82542, 83921 when specified as PFAS testing based on diagnosis, considered INV&NMN | April 1, 2025 | *MED.00150 Hepzato Kit™ (melphalan hepatic delivery system) | Outlines the MN and INV&NMN criteria for Liver‑directed administration of high‑dose melphalan (Hepzato Kit) Added existing HCPCS and ICD‑10-PCS codes J9248, XW053T9 and CPT 93799 NOC, considered MN when criteria are met | April 1, 2025 | *DME.00052 Brain Computer Interface Rehabilitation Devices | Brain computer interface rehabilitation devices, including but not limited to electroencephalography (EEG)‑driven upper extremity powered exercisers, are considered INV&NMN Existing HCPCS code E0738 effective 4/1/2024 for IpsiHand is considered INV&NMN for all indications | April 1, 2025 | *LAB.00051 Per‑ and Polyfluoroalkyl Substances PFAS Testing | Testing for PFAS substances is considered INV&NMN for all indications Existing CPT PLA codes 0394U, 0457U for PFAS tests, and codes 82542, 83921 when specified as PFAS testing based on diagnosis, considered INV&NMN | April 1, 2025 |
Below are the current Medical Policies and/or Clinical Guidelines that have been approved.* Denotes prior authorization required Policy/guideline | Information | Effective date | CG‑MED-46 Ambulatory Electroencephalography (Previously titled: Electro‑encephalography and Video Electroencephalographic Monitoring) | Revised title Removed attended video EEG monitoring in a healthcare facility from scope of document Removed ICD‑10-PCS code 4A10X4Z for inpatient monitoring, no longer applicable | October 1, 2024 | CG‑SURG-83 Bariatric Surgery and Other Treatments for Clinically Severe Obesity | Updated ICD‑10-CM diagnosis codes, added E66.811‑E66.813, E88.82, Z68.56 | October 1, 2024 | *DME.00011 Electrical Stimulation as a Treatment for Pain and Other Conditions: Surface and Percutaneous Devices | Revised INV&NMN statement, adding external lower extremity nerve stimulator Added new HCPCS codes A4543, E0721 for Sparrow device, A4544, E0743 for TOMAC device effective 10/1/2024, all considered INV&NMN | April 1, 2025 | *DME.00012 Intrapulmonary Percussive Ventilation Devices | Added new HCPCS codes A7021, E0469 effective 10/1/2024 for Volara system considered INV&NMN (replacing E1399 NOC) | April 1, 2025 | *LAB.00003 In Vitro Chemosensitivity Assays and In Vitro Chemoresistance Assays | Added new CPT PLA code 0511U effective 10/1/2024 for PARIS test considered NMN | April 1, 2025 | *LAB.00015 Detection of Circulating Tumor Cells | Added new CPT PLA codes 0490U, 0491U, 0492U effective 10/1/2024 for CELLSEARCH tests, considered INV&NMN | April 1, 2025 | *LAB.00026 Systems Pathology and Multimodal Artificial Intelligence Testing for Cancerous and Precancerous Conditions (Previously titled: Systems Pathology and Multimodal Artificial Intelligence Testing for Prostate Cancer) | Revised title Added precancerous lesions with Barrett’s esophagus as an example to Position Statement Added existing CPT PLA code 0108U for TissueCypher Barrett's Esophagus Assay, considered INV&NMN | April 1, 2025 | *LAB.00033 Protein Biomarkers for the Screening, Detection and Management of Prostate Cancer | Added new CPT PLA code 0495U effective 10/1/2024 for Stockholm3 test considered INV&NMN | April 1, 2025 | *LAB.00040 Serum Biomarker Tests for Risk of Preeclampsia | Revised diagnosis with diagnose in the INV&NMN statement Added new CPT PLA code 0482U effective 10/1/2024 for preeclampsia test considered INV&NMN | April 1, 2025 | *LAB.00046 Testing for Biochemical Markers for Alzheimer's Disease | Codes 0445U, 0459U will be considered MN when criteria met for leqembi therapy; added new CPT PLA codes 0479U, 0503U effective 10/1/2024 for pTau and blood testing considered INV&NMN | April 1, 2025 | *LAB.00050 Metagenomic Sequencing for Infectious Diseases in the Outpatient Setting | Added new CPT PLA code 0480U effective 10/1/2024 for Mayo Clinic metagenomic test considered INV&NMN | April 1, 2025 | *MED.00134 Non‑invasive Heart Failure and Arrhythmia Management and Monitoring Systems (Previously titled: Non‑invasive Heart Failure and Arrhythmia Management and Monitoring System) | Revised title Revised Position Statement to remove device name and change from singular to plural devices No specific codes for new devices AVIVO, VitalConnect, Zoe systems & BodyPort scale considered INV&NMN, added existing code 93701 (non‑specific) and E1399 NOC | April 1, 2025 | *MED.00135 Gene Therapy for Hemophilia | Added new HCPCS code C9172 effective 10/1/2024 for Beqvez considered MN when criteria are met | April 1, 2025 | *MED.00140 Gene Therapy for Beta Thalassemia | Added new MN statement regarding autologous hematopoietic stem cell mobilization and pheresis Added codes 38206, 38232, 38241, 6A550ZV, 6A551ZV for autologous stem cell procedures, MN when criteria are met for gene therapy | April 1, 2025 | *MED.00142 Gene Therapy for Cerebral Adrenoleuko‑dystrophy | Added new MN statement regarding autologous hematopoietic stem cell mobilization and pheresis Added codes 38206, 38232, 38241, 6A550ZV, 6A551ZV for autologous stem cell procedures, MN when criteria are met for gene therapy | April 1, 2025 | *MED.00144 Gene Therapy for Duchenne Muscular Dystrophy | Revised wording in the INV&NMN statement to include the brand name (ELEVIDYS) and remove the phrase for all other indications, including Removed NOC codes C9399, J3490, J3590 no longer applicable | October 1, 2024 | *MED.00146 Gene Therapy for Sickle Cell Disease | Added new MN statement regarding autologous hematopoietic stem cell mobilization and pheresis Added codes 38206, 38232, 38241, 6A550ZV, 6A551ZV for autologous stem cell procedures, MN when criteria are met for gene therapy | April 1, 2025 | *MED.00148 Gene Therapy for Metachromatic Leukodystrophy | Added new MN statement regarding autologous hematopoietic stem cell mobilization and pheresis Added codes 38206, 38232, 38241, 6A550ZV, 6A551ZV for autologous stem cell procedures, MN when criteria are met for gene therapy | April 1, 2025 | *SURG.00011 Allogeneic, Xenographic, Synthetic, Bioengineered, and Composite Products for Wound Healing and Soft Tissue Grafting | Added new HCPCS codes A2027, A2028, A2029, Q4334, Q4335, Q4336, Q4337, Q4338, Q4339, Q4340, Q4341, Q4342, Q4343, Q4344, Q4345 effective 10/1/2024 for products considered INV&NMN | April 1, 2025 | *SURG.00023 Breast Procedures; including Reconstructive Surgery, Implants and Other Breast Procedures | Added new ICD‑10-PCS codes 0HRT07B, 0HRU07B, 0HRV07B effective 10/1/2024 for lumbar artery perforator flap for breast reconstruction when criteria are met | October 1, 2024 | *SURG.00032 Patent Foramen Ovale and Left Atrial Appendage Closure Devices (Previously titled: Patent Foramen Ovale and Left Atrial Appendage Closure Devices for Stroke Prevention) | Revised title Revised MN statement Added NMN statements for PFO and LAAA closure Added an INV&NMN statement for PFO Revised coding section to indicate PFO and LAAA codes considered NMN when criteria not met (were Inv&NMN) | October 1, 2024 | *SURG.00047 Transendoscopic Therapy for Gastroesophageal Reflux Disease, Dysphagia or Gastroparesis (Previously titled: Transendoscopic Therapy for Gastroesophageal Reflux Disease, Dysphagia and Gastroparesis) | Revised title Changed the word and to or in the INV&NMN statement Added ICD‑10-CM Q39.5 considered MN for POEM procedure when criteria are met | October 1, 2024 | *SURG.00121 Transcatheter Heart Valve Procedures | Added new ICD‑10-PCS code X2RJ3RA effective 10/1/2024 for tricuspid valve replacement procedure considered INV&NMN | October 1, 2024 | *SURG.00128 Implantable Left Atrial Hemodynamic Monitor | Added new CPT Category III codes 0933T, 0934T effective 1/1/2025, considered INV&NMN | April 1, 2025 | *SURG.00129 Oral, Pharyngeal and Maxillofacial Surgical Treatment for Obstructive Sleep Apnea or Snoring | Added existing CPT code 64568 for new single‑lead Inspire upper airway HNS, MN when criteria are met | April 1, 2025 | *SURG.00135 Renal Sympathetic Nerve Ablation | Added ICD‑10-PCS X05133A effective 10/1/2024 and CPT Category III code 0935T effective 1/1/2025 for renal nerve ablation considered INV&NMN; removed non‑specific code 015M3ZZ | April 1, 2025 | *SURG.00153 Cardiac Contractility Modulation Therapy | Added new CPT Category III codes 0915T‑0931T effective 1/1/2025 for CCM plus CD considered INV&NMN | April 1, 2025 | *TRANS.00010 Autologous and Allogeneic Pancreatic Islet Cell Transplantation | Added new ICD‑10-PCS code XW033DA effective 10/1/2024 for Lantidra, considered INV&NMN | October 1, 2024 | *TRANS.00024 Hematopoietic Stem Cell Transplantation for Select Leukemias and Myelodysplastic Syndrome | Updated ICD‑10-CM diagnosis codes, added C83.0A, C83.5A effective 10/1/2024 | October 1, 2024 | *TRANS.00028 Hematopoietic Stem Cell Transplantation for Hodgkin Disease and non‑Hodgkin Lymphoma | Updated ICD‑10-CM diagnosis codes, added C81.9A, C85.9A, C86.61 effective 10/1/2024 | October 1, 2024 | *TRANS.00038 Thymus Tissue Transplantation | Added existing code J3590 NOC being used for RETHYMIC, replacing L8699 | October 1, 2024 |
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CM-074049-24 Effective January 5, 2024 The Medical Policies, Clinical Utilization Management (UM) Guidelines, and Third-Party Criteria below were developed and/or revised during Quarter Two, 2024. Note, several policies and guidelines were revised to provide clarification only and are not included. Some may have expanded rationales, medical necessity indications, or criteria, and some may involve changes to policy position statements that might result in services that previously were covered being found to be not medically necessary. Please share this notice with other providers in your practice and office staff. To view a guideline, visit the Criteria Search Page. Notes/updatesUpdates marked with an asterisk (*) notate that the criteria may be perceived as more restrictive: - MED.00148 Gene Therapy for Metachromatic Leukodystrophy:
- Outlines the Medically Necessary and Not Medically Necessary criteria for gene therapy for metachromatic leukodystrophy
Medical PoliciesOn May 9, 2024, the Medical Policy and Technology Assessment Committee (MPTAC) approved the following Medical Policies. These medical policies take effect January 5, 2025. Publish date | Medical Policy number | Medical Policy title | New or revised | May 16, 2024 | *MED.00148 | Gene Therapy for Metachromatic Leukodystrophy | Revised |
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-068820-24-CPN68231 - Coupe Health offers a unique plan starting January 2025 with upfront service pricing and zero‑interest installments.
- Providers receive full contracted rates without needing to collect payments directly from patients.
- Members identify with co‑branded ID cards, and claims processing remains consistent with existing procedures.
Beginning in January 2025, we are partnering with Coupe Health to offer members an alternative health plan that provides price certainty, easy access to quality care, and a seamless user experience. With Coupe Health, members know the price of medical services upfront and can pay for their care in zero‑interest installments. They pay nothing at the time of service and receive a single statement at the end of the month for all covered services. Care providers are paid their contracted rate in full — without any deduction for patient responsibility. This means you can focus on providing care to your patients without the need to collect payments or track down debt. How does Coupe Health work? - Same quality network: Your patients can access our BlueCard® PPO Network.
- Price certainty: Your patients will know the cost of all covered medical services and will pay $0 upon their visit.
- Focus on care: You’ll be paid your contracted rate in full — allowing you and your staff to focus on patient care, not payment collection.
How do I know if my patient has a Coupe Health medical plan or is eligible for one? Members with a Coupe Health medical plan will have a co‑branded ID card — Our logo will be in the top‑left corner, and the Coupe Health logo will be in the top‑right corner: 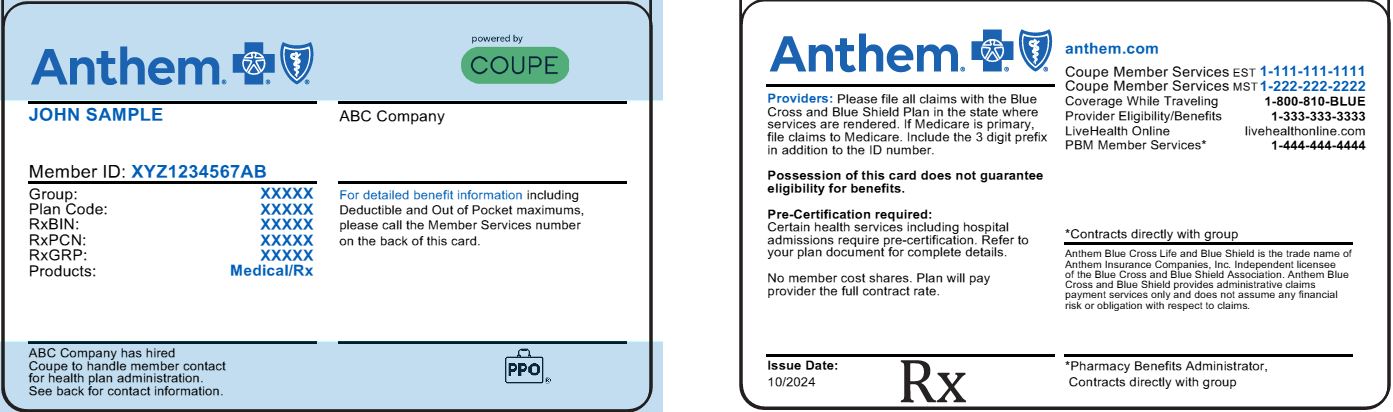
- Our PPO (or Select) will be the network listed on the card.
- Coupe Health plans will be available in select states beginning in January 2025, through a member’s employer.
Is there a different process for filing claims? - No. Coupe Health claims are processed as our claims, and you will use the same prefix on your patient’s member ID card and our same payer ID.
- Some members may opt into a Coupe Health plan that requires them to pay at the time of service. This will be reflected in the EDI inquiry file.
Coupe Health will be available to select individual and family plan members beginning in January 2025. For more information, visit https://www.coupehealth.com/providers/ or contact your Provider Services representative. We are committed to helping patients more easily access the care they need. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CM-070358-24 To view the 2025 benefits and changes for the Federal Employees Health Benefits (FEHB) and Postal Service Health Benefits (PSHB) programs, go to fepblue.org. Select Get Support & Resources > Brochures & Resources. Here you will find the plan brochures, benefit plan summaries, and quick reference guides for 2025. If you have questions, please contact Customer Service at: California — FEHB: 800‑284-9093 or PSHB: 833‑821-2287 Colorado — FEHB: 800‑852-5957 or PSHB: 833‑821-2313 Connecticut — FEHB: 800‑438-5356 or PSHB: 833‑821-2261 Georgia — FEHB: 800‑282-2473 or PSHB: 833‑821-2257 Indiana — FEHB: 800‑382-5520 or PSHB: 833‑821-1958 Kentucky — FEHB: 800‑456-3967 or PSHB: 833‑821-1960 Maine — FEHB: 800‑722-0203 or PSHB: 833‑821-2263 Missouri — FEHB: 800‑392-8043 or PSHB: 833‑821-1966 Nevada — FEHB: 800‑727-4060 or PSHB: 833‑821-2325 New Hampshire — FEHB: 800‑852-3316 or PSHB: 833‑821-2286 New York — FEHB: 800‑522-5566 or PSHB: 833‑821-2256 Ohio — FEHB: 800‑451-7602 or PSHB: 833‑821-1970 Virginia — FEHB: 800‑552-6989 or PSHB: 833‑821-2258 Wisconsin — FEHB: 800‑242-9635 or PSHB: 833‑821-2245 Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CM-075158-24 Effective January 1, 2025, and upon member consent, specialty pharmacy prescriptions for Medicare members currently being dispensed by CarelonRx Specialty Pharmacy will be transferred to BioPlus Specialty Pharmacy. What happens next?- Medicare patients received a letter in November explaining this transition. If they provide consent to move to BioPlus, they will receive a phone call from BioPlus to review important information related to their prescriptions.
- If you have Medicare patients who choose to move their prescription, BioPlus will contact you to request new prescriptions, refills, or prior authorizations.
- If you have Medicare patients who choose not to move their prescription, no action is required.
Benefits of working with BioPlusIf your Medicare patients choose to move to BioPlus, here is what you can expect: - Faster approvals:
- Know in two hours whether your patient’s medication will be filled
- Less paperwork and hassle over benefits verification and appeals
- More help with securing patient financial assistance
CarelonRx, Inc. and BioPlus work together to deliver patients an unparalleled level of high‑tech, high‑touch service that focuses on their whole health. If you have questions, contact your provider relationship management representative or BioPlus directly at 833‑549-2874. Through genuine collaboration, we can simplify access to care and help you deliver high‑quality, equitable healthcare. CarelonRx, Inc. is an independent company providing pharmacy benefit management services on behalf of the health plan. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-072475-24-CPN72385 Our pharmacy benefit management partner, CarelonRx Inc., has acquired Kroger Specialty Pharmacy. This follows the recent acquisitions of BioPlus Specialty Pharmacy, all aimed at enhancing support for individuals with chronic and complex conditions. To ensure a seamless patient experience, most prescriptions for former Kroger Specialty Pharmacy patients are being handled by BioPlus Specialty Pharmacy, a CarelonRx company. If you have new specialty pharmacy prescriptions, please send them to BioPlus Specialty Pharmacy. If you have any questions, please call your provider relationship management representative. With your help, we can continually build towards a future of shared success. CarelonRx, Inc. is an independent company providing pharmacy benefit management services on behalf of the health plan. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-072480-24-CPN72372 The CarelonRx, Inc. weight management program offers support and advocacy for patients throughout their weight loss journey. Individuals who are at least 18 years of age with a BMI of at least 27 have access to personalized weight management from CarelonRx through their partner, Lark. CarelonRx’s weight management program will provide access to digital coaching and wellness tools to help participants manage and monitor their weight goals. Patients benefit from 24/7 digital connectivity and access to personalized coaching support whenever needed. Patients design their own journey with goals and missions to inform personalized wellness plans to ensure a holistic experience. What your patients can expect:- Engagement in lifestyle support through the Lark mobile app, which includes diet, exercise, and nutrition
- Behavioral health support and ongoing social drivers of health (SDOH) monitoring
- Injection, adherence, and side effect support for those on a GLP‑1 for weight loss
- Ongoing weight maintenance support tailored to individual weight loss goals
Take actionIf a prior authorization (PA) is requested, you will be asked to confirm the member's enrollment in the Lark Weight Management Program. For more information about the program, members can: - Visit Anthem.com or the Sydney mobile app.
- Call the customer service number on the back of their identification card.
CarelonRx, Inc. is a separate company providing utilization review services on behalf of the health plan. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CM-075184-24 Prior authorizationEffective for dates of service on or after March 1, 2025, the specialty Medicare Part B drug listed in the table below will be included in our precertification review process. Federal and state law, as well as state contract language and CMS guidelines, including definitions and specific contract provisions/exclusions, take precedence over these precertification rules and must be considered first when determining coverage. Noncompliance with new requirements may result in denied claims. HCPCS or CPT® codes | Medicare Part B drugs | C9399, J3590 | Eylea (aflibercept) biosimilars:
Ahzantive (aflibercept‑mrbb)
Enzeevu (aflibercept‑abzv)
Opuviz (aflibercept‑yszy)
Pavblu (aflibercept‑ayyh)
Yesafili (aflibercept‑jbvf) | C9399, J9999 | Lymphir (denileukin diftitox‑cxdl) | C9399, J3590 | Niktimvo (axatilmab‑csfr) | C9399, J3590 | Nypozi (filgrastim‑txid) | J3590 | Ocrevus Zunovo (ocrelizumab/hyaluronidase‑ocsq) | C9399, J9999 | Rytelo (imetelstat) | C9399, J9999 | Tecelra (afamitresgene autoleucel) | J3590 | Yimmugo (immune globulin intravenous, human‑dira) |
Step therapyEffective March 1, 2025, the following Part B medications from the current Clinical Criteria Guidelines will be included in our medical step therapy precertification review process. Step therapy review will apply upon precertification initiation, in addition to the current medical necessity review (as is current procedure). Step therapy will not apply for members who are actively receiving medications listed below. Clinical Criteria Guidelines are publicly available on the provider website. Visit the Clinical Criteria page to search for specific criteria. Clinical UM Guidelines | Status | Drug(s) | CC‑0002 | Non‑preferred | Nypozi (filgrastim‑txid) | CC‑0003 | Non‑preferred | Yimmugo (immune globulin intravenous, human‑dira) |
Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-072452-24-CPN72386 Effective for dates of service on or after April 1, 2025, the specialty Medicare Part B drug listed in the table below will be included in our precertification review process. Federal and state law, as well as state contract language and CMS guidelines, including definitions and specific contract provisions/exclusions, take precedence over these precertification rules and must be considered first when determining coverage. Noncompliance with new requirements may result in denied claims. HCPCS or CPT® codes | Medicare Part B drugs | J1952 | Camcevi (leuprolide mesylate) | J0175 | Kisunla (donanemab‑azbt) | J3590 | Piasky (crovalimab‑akkz) | J3590, J9999 | Tevimbra (tislelizumab‑jsgr) | C9399, J3590 | Tyenne (tocilizumab‑aazg) |
Notification of Specialty Pharmacy Medical Step Therapy updatesEffective February 1, 2025, the following Part B medications from the current Clinical Criteria Guidelines will be included in our medical step therapy precertification review process. Step therapy review will apply upon precertification initiation, in addition to the current medical necessity review (as is current procedure). Step therapy will not apply for members who are actively receiving medications listed below. Clinical UM Guidelines are publicly available on the provider website. Visit the Clinical Criteria page to search for specific criteria. Clinical UM Guidelines | Preferred drug(s) | Nonpreferred drug(s) | CC‑0003 | Intravenous: Gamunex‑C1 Octagam Subcutaneous: Cutaquig Hizentra Xembify | Intravenous: Alyglo Asceniv Bivigam Flebogamma DIF Gammaked1 Gammagard1 Gammagard S/D Gammaplex Panzyga Privigen Subcutaneous: Cuvitru HyQvia |
1 Gamunex‑C,Gammaked, and Gammagard may be administered intravenously or subcutaneously. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-071026-24-CPN70592 On October 11, 2024, Pine Pharmaceuticals, the largest producer of repackaged bevacizumab (Avastin®), communicated that it would no longer be a supplier of repackaged, prefilled bevacizumab syringes. Our preferred products include Avastin, Byooviz, Cimerli, Eylea, Eylea HD, Lucentis, and Vabysmo. To avoid access issues or treatment delays for members receiving this treatment, we encourage providers to reach out if necessary to our prior authorization department for an alternative antivascular endothelial growth factor drug for our members. All expedited requests for a Part B drug will have a determination made and the enrollee will be notified of the decision as expeditiously as the enrollee’s health condition requires, but no later than 24 hours after the request is received. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. PCTS-1044-1, MULTI-ALL-CR-075366-24 At a glance: - Care providers must prepare for HEDIS® medical record reviews starting January 2025.
- Care providers will submit records through Remote Electronic Medical Record (EMR) Access Service, website upload, fax, secure file transfer protocol (SFTP), mail, or on-site.
BackgroundEach year, we perform a review of a sample of our members’ medical records as part of the HEDIS quality study. HEDIS is part of a nationally recognized quality improvement initiative and is used by the Centers for Medicare & Medicaid Services (CMS), the National Committee for Quality Assurance (NCQA), and several states to monitor the performance of managed care organizations. We will begin requesting medical records in January 2025. No special authorization is needed for you to share member medical record information with us since quality assessment and improvement activities are routine parts of healthcare operations. Ways to submit your records, listed in our preferred order:- Remote EMR Access Service: We offer the Remote EMR Access Service to care providers to submit member medical record information to us. If you are interested in more information, contact us at Centralized_EMR_Team@anthem.com.
- Upload: Medical records can be uploaded to our secure website using the instructions in the request document.
- Fax: Medical records can be faxed to us using the instructions in the request document.
- SFTP: Medical records can be uploaded via a secure website.
- U. S. Postal Service: Medical records can be mailed to us using the instructions in the request document.
- On-site: Medical records can be pulled by a representative at your local office where medical records are located.
HEDIS review is time sensitive, so submit the requested medical records within the timeframe indicated in the initial HEDIS request document. We appreciate the care you provide to our members. Your assistance is crucial to ensuring our data is statistically valid, auditable, and accurately reflects quality performance. Contact us
Availity Chat with Payer is available during normal business hours. Get answers to your questions about eligibility, benefits, authorizations, claims status, and more. To access Availity Essentials, go to https://Availity.com and select the appropriate payer space tile from the drop-down. Then, select Chat with Payer and complete the pre-chat form to start your chat.
For additional support, visit the Contact Us section of our provider website for the appropriate contact. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). Anthem Blue Cross and Blue Shield Medicaid is the trade name of Anthem Kentucky Managed Care Plan, Inc. Anthem Blue Cross and Blue Shield is the trade name of Anthem Health Plans of Kentucky, Inc. Independent licensee(s) of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. KYBCBS-CDCRCM-071172-24-CPN71157 |
