Provider News VirginiaSeptember 1, 2020 September 2020 Anthem Provider News - VirginiaState & FederalState & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 Discharge planning
In mid-June 2020, Anthem Blue Cross and Blue Shield in Virginia and our affiliate HealthKeepers, Inc. notified all professional providers about upcoming contract changes to include updates to fee schedules, reimbursement policies and the provider manual.
The amendment is automatically effective on October 1, 2020.
Provider Contract and Fee Schedule Notifications via Availity
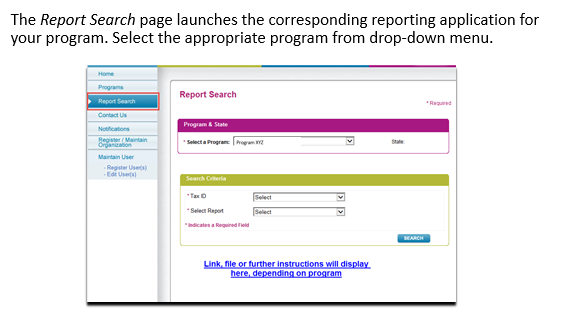
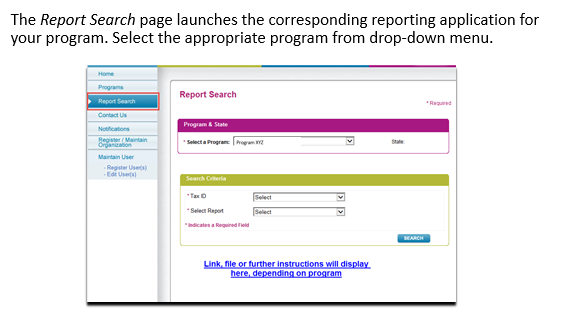
In the June 2020 Provider News, we announced the release of Provider Contract and Fee Schedule Notifications via Availity – our secure, Web-based provider tool. With this new automated process, when Anthem notifies you in writing of a statewide fee schedule update or provider contract amendment, you can log into Availity any time to securely access and download a digital copy of your amendment documents using the Provider Online Reporting tool in Availity.
As a reminder, please take time today to view your contract amendment documents via Availity’s Provider Online Reporting tool if you have not already done so. Keep in mind that only authorized users in your practice or facility can view the confidential contract amendments using the reporting tool. Your Availity administrator must grant access to the reporting tool if you do not currently have access. For easy reference, we’re again including the information below to help you get started with Provider Contract and Fee Schedule Notifications if needed.
Provider Online Reporting Reference Guide: How to get started
This document will familiarize you with the Provider Online Reporting application found on the Availity Portal. Using our web-based reporting application, you will be able to access regularly updated reports.
- For Availity Administrators – How to assign access
- For Users – How to navigate to the reports
If your organization is not currently registered for the Availity Portal, go to www.availity.com and select Register to complete the online application.
Your Administrator will need to take the following steps to assign access to Provider Online Reporting:
- Assign the user role of Provider Online Reporting to your Availity access.
- Select Payer Spaces in the navigation bar and then choose the payer tile that corresponds to the market.
- Accept the User Agreement (once every 365 days).
- On the Applications tab, select Provider Online Reporting.
- Choose the organization and select Submit.
- In the Provider Online Reporting application, register the tax ID by selecting Register/Maintain Organization.
- Last, register users to the program by selecting Register Users and completing the required fields.
Accessing reports:
- After logging in to Availity, select Payer Spaces in the navigation bar and then choose the payer tile that corresponds to the market.
- Accept the User Agreement (once every 365 days).
- On the Applications tab, select Provider Online Reporting.
- Choose the organization and select Submit.
- Select Report Search, choose the type of report, and then launch your program’s reporting application.


Looking ahead
Going forward, you’ll no longer receive from us large printed paper mailings or CDs in the mail regarding contract amendment changes as in the past. We hope this new streamlined process via Availity better supports you in quickly and easily accessing critical business information at your fingertips that impacts your business interactions with us – saving you time.
For further assistance with Availity, please contact Availity Client Services at 1-800-282-4548.
If you have questions about the amendment process, please contact your Anthem Network Manager. View the Anthem contact list online at anthem.com.
631-0920-PN-VA Anthem Blue Cross and Blue Shield and our affiliate HealthKeepers, Inc. have implemented necessary requirements to comply with Virginia legislative House Bill (HB) 822 that became effective July 1, 2020. If you are a new provider applicant under credentialing review for participation in provider networks offered by Anthem and HealthKeepers, Inc., HB822 allows you to see Anthem members and retroactively receive payments if you are ultimately credentialed.
This means that as of July 1, 2020, if you are a provider who already has an executed contract, and submits a completed credentialing application to us, Anthem and HealthKeepers, Inc. will adhere to the requirements specified in HB 822. If you are a provider entering into a new contract, the effective date will be determined based on the latter of the contract execution date, or the completed credentialing application receipt date. Requirements in the bill do not apply to credentialing applications submitted BEFORE July 1, but which are still in the credentialing review process after the July effective date.
Under the new law, we are required to establish protocols and procedures for reimbursing new provider applicants at the contracted in-network rate for approved, covered services provided during the period in which a provider’s credentialing application is pending. Effective July 1 under HB 822, the credentialing period begins with the receipt of a completed credentialing application. Incomplete credentialing applications and denied applications are excluded.
What lines of our business are impacted?
Members enrolled in the following health benefit plans are impacted by the new state legislation:
- Anthem's PAR/PPO health benefit plans.
- HealthKeepers, Inc.'s Anthem HealthKeepers (commercial, non-Medicaid) health benefit plans. This includes health plans members purchase on or off the Health Insurance Marketplace (commonly referred to as the exchange).
- Commonwealth of Virginia COVA Care and COVA HDHP health benefit plans, the Local Choice (TLC) health benefit plans, and the Line of Duty (LODA) health benefit plans.
- Medicare Supplement health benefit plans.
Those lines of our business NOT impacted are:
- Blue Cross and Blue Shield Service Benefit Plan (also called the Federal Employee Program or FEP).
- Administrative services only (ASO) health plans.
- HealthKeepers, Inc.'s Anthem HealthKeepers Plus/FAMIS (Medicaid) health plans.
- Medicare Advantage health plans.
Impact to providers: Call to action
Once the effective date is determined, the effective date will apply to all lines of business; however, based on the line of business, claims will process differently.
Hold claims for Anthem members: During the credentialing period, providers are required to hold claims for our members until Anthem sends a final notification of a credentialing decision. If you submit claims to Anthem during the credentialing period before receiving a credentialing decision, claims for the impacted lines of business noted above will be rejected indicating that the claims must be resubmitted upon a final credentialing decision. Members will be protected from inappropriate billing and held harmless during this period. However, for lines of business not impacted by legislation, claims submitted before receiving a credentialing decision will process on out-of-network benefits based on the member’s policy. Submitting claims too early may result in inappropriate payments and member cost shares.
Patient financial responsibility: Upon receiving notice of Anthem's final credentialing approval, providers may collect any applicable member cost shares based on members' health benefit plans as appropriate. Providers with approved credentialing applications are required to submit claims under their contract with Anthem and HealthKeepers, Inc. Those with denied applications, while not obligated to so do, are encouraged to file claims to us on behalf of members to help speed claims processing and payments as appropriate. As always, we encourage you to verify eligibility and benefits for members via our secure Web-based provider tool – Availity.
Notify Anthem members as required by HB 822: In order to submit claims pursuant to HB 822, providers are required to take the following actions regarding members enrolled in health benefit plans offered by Anthem and HealthKeepers, Inc.:
- Notify members – either in writing or electronically – stating that the provider’s credentialing application has been submitted to Anthem and is under review.
- Provide the notice in advance of providing treatment to members.
- Include in the notice to members certain credentialing information as outlined in HB 822. Please refer to the legislation for actual requirements and how they impact you.
Questions
If you have questions about the status of your credentialing application, please email our credentialing area at credentialing@anthem.com. All other questions about the credentialing process should be directed to your Anthem network manager.
Please forward this information to those in your practice who may need this information.
610-0920-PN-VAAnthem Blue Cross and Blue Shield will begin publishing new indicators in our online provider directories to help members easily identify facilities and physicians designated as medication assisted treatment (MAT) providers for opioid use disorder.
These directory indicators fall into four categories related to MAT:
- Facility that provides MAT
- Physician who provides MAT
- Facility with a certified opioid treatment program
- Facility that provides counseling for opioid use disorders
We encourage facilities and individual providers who provide these services to update their demographic information so these MAT indicators can be added to our directories. To submit updated professional demographic information, please visit anthem.com and locate the Provider Maintenance Form to submit changes to your information. For facility updates, please contact your provider network representative. Please contact Provider Services if you have any questions.
630-0920-PN-VA Migrate your electronic data interchange (EDI) transactions to Availity today. As a reminder, the Availity migration continues full speed ahead. Anthem Blue Cross and Blue Shield will guide you to make it an effortless transition without having to rush.
If you, your clearinghouse or vendor have already migrated to Availity, thank you. You are a step ahead. If not, please start the process today to make the transition before September 15, 2020.
Take Action Now! Availity setup is simple and at no cost for you.
Learn about Availity to get started today:
All EDI transmissions currently sent or received today via the Anthem gateway are now available on the Availity EDI Gateway.
- 837 Institutional and Professional
- 835 Electronic Remittance Advice
- 270/271 Eligibility Request
- 278 Prior Authorization/Referrals
- 278N Inpatient Admission and Discharge Notification
Below are the options you can choose from to exchange EDI transmissions with the Availity EDI Gateway:
- Transition your existing connection with Anthem and become a direct submitter with Availity.
- Use your existing Clearinghouse or Billing Company for your EDI transmissions. (Work with them to ensure connectivity to the Availity EDI Gateway).
- Use Direct Single Claim entry through the Availity Portal with the new attachment function
Share with your team what you learn
Enroll in one of Availity’s free courses and training demos at your convenience. Making the switch to Availity's EDI Gateway is easy if you have all the resources that you need.
Follow these steps to register with Availity
- Log in and select Help & Training | Get Trained to open the Availity Learning Center in a new tab Search Catalog field and choose. It is your dedicated ALC account.
- Search by keyword (Medical Attachments/Attachments) to find on-demand and live training options.
- Click Enroll to enroll for a course and then go to your Dashboard to access it any time.
For questions, contact Availity Client Services at 1-800-Availity (1-800-282-4548) for assistance Monday - Friday, 8 a.m. - 7 p.m. ET.
635-0920-PN-VAPatient360 is a dashboard you can access through the Availity Portal that gives you a full 360° view of your patients’ health and treatment histories and will help you facilitate care coordination. You can drill down to specific items in the medical records of your patients who are enrolled in Anthem health benefit plans to retrieve demographic information, care summaries, claims details, authorization details, pharmacy information, and care management-related activities.
What’s new
Medical providers now have the option available to include feedback for Anthem patients who have gaps in care. Your practice can locate these care gaps in the Active Alerts section on the Member Care Summary page of the Patient360 application.
Once you have completed the required fields on the Availity Portal to access Patient360 you will land on the Member Summary page of the application. To provide feedback, select the Clinical Rules Engine (CRE) within the Active Alerts section. This will open the Care Gap Alert Feedback Entry window. You can choose the feedback menu option that applies to your patient’s care gap.
Are you using Patient360 for the first time? You can easily access Patient360 on the Availity Portal.
First, you need to be assigned to the Patient360 Role which your Availity Administrators can locate within the Clinical Roles options.
Once you have the Availity role assignment, navigate to Patient360 through the Availity Portal by selecting the application on Anthem Payer Spaces or by choosing the Patient360 link located on the patient’s benefits screen.
Job aid to help you get started
The Patient360 Navigation Overview illustrates the steps to access Patient360 through the Availity Portal, and instructions on how to provide feedback for your patients who are displaying a Care Gap Alert. This reference is available for you to access online through the Custom Learning Center.
- From Availity’s home page, select Payer Spaces | Anthem payer tile| Applications | Custom Learning Center.
- Select Resources from the menu located on the upper left corner of the page. (To use the catalog filter to narrow the results select Payer Spaces from the Category menu.)
- Select Download to view and/or print the reference guide.
641-0920-PN-VA Anthem Blue Cross and Blue Shield now offers a full suite of options to assist with medical record submissions. To ease your administrative burden and recognizing your staff may be working remotely, we have increased the intake channels for required medical records supporting claim submissions.
Options available to you
Leverage any of the following Availity-hosted channels for electronic claim attachment transmission:
|
EDI Transaction: X12 275 Patient Information (version 5010)
|
Anthem supports the industry standard X12 275 transaction for electronic transmission of supporting claims documentation including medical records (pdf, jpeg, tif file types) Access your X12 275 companion guide for more details.
Electronic Integrated Submission – Submit the claim via EDI 837 batch file and supporting documentation via x12 275.
|
|
Availity Secure Provider Portal Options
|
Direct Data Entry (DDE) – The direct data entry claim application allows you to upload supporting documentation for a defined claim (unsolicited process).
Attachments – New tool – Submit solicited or unsolicited supporting documentation for your claims.
|
Attend an Availity hosted webinar to learn more about all capabilities
Start your transition today
Start now to adopt these new processes and experience the many advantages to using an electronic option for claim attachment submission. You may find you are able to use these new processes to replace your more manual processes of submitting supporting documentation via fax or mail (United States Postal Service).
Advantages:
- Easy Submission of medical documentation to include but not limited to:
|
Itemized bills
|
|
Medical records
|
|
Discharge summaries
|
- Less administrative burden – Medical records submitted electronically save an average of 4 minutes per record for staff versus faxing or mailing your records in.
- Electronic acknowledgment with a transaction audit trail – Confirm delivery/receipt.
- Comprehensive history – View past medical record submissions by your organization.
- Administrative savings – Reduce your mailing expense and/or fax related expenses.
Want to learn more?
Register for an upcoming webinar session
- In Availity Portal, select Help & Training > Get Trained.
- The Availity Learning Center opens in a new browser tab.
- Search for and enroll in a session using one of these options.
- In the Catalog, search by webinar title or keyword (medattach).
- Select the Sessions tab to scroll the live session calendar.
- After you enroll, you’ll receive emails with instructions to join the session.
September/October Webinar Dates
|
Date
|
Day
|
Time
|
|
September 10, 2020
|
Thursday
|
11 a.m. – Noon ET
|
|
September 21, 2020
|
Monday
|
Noon – 1 p.m. ET
|
|
October 7, 2020
|
Wednesday
|
4 p.m. – 5 p.m. ET
|
|
October 20, 2020
|
Tuesday
|
11 a.m. – Noon ET
|
636-0920-PN-VA
On September 12, 2020, we are introducing Interactive Care Reviewer (ICR) for our members enrolled in Anthem’s Commercial lines of business. (This includes Commercial plans offered by our affiliate, HealthKeepers, Inc.) You will access ICR through the Availity Portal.
At this time, ICR will be available as your self-service online authorization tool for new medical and behavioral health prior authorization requests. You will be able to submit authorization requests, check case status, update cases and request clinical appeals.
Beginning September 12, you will no longer be able to use Point of Care to initiate authorization requests for these members.
On August 15, 2020, we introduced ICR for members enrolled in the Blue Cross and Blue Shield Service Benefit Plan (commonly referred to as the Federal Employee Program® or FEP). ICR is now your exclusive online tool for these authorization requests.
On October 17, 2020, the Point of Care secure web portal will be retired. You will be able to check status and update all authorizations that were previously submitted through Point of Care using the ICR tool.
Ask your Availity administrator to grant you the required ICR role assignment now so you can begin using the tool immediately when it becomes available.
- Do you create and submit prior authorization requests?
Authorization and Referral Request role assignment
- Do you check the status of the case or results of the authorization request?
Authorization and Referral Inquiry role assignment
When ICR is launched, follow these steps to navigate to ICR through Availity to request and check the status of prior authorizations
- Select Patient Registration from Availity’s home page
- Select Authorizations & Referrals
- Select Authorizations (for requests) | Select Auth/Referral Inquiry (for inquiries)
Register for our September webinar
We offer training every month to familiarize new users with ICR features and navigation of the tool. REGISTER to attend a September webinar.
Additional ICR resources are available through the Custom Learning Center
Follow the steps outlined below to access self-paced videos located on the Custom Learning Center. From Availity’s home page, select Payer Spaces | Anthem tile | Applications | Custom Learning Center
|
STEP
|
INSTRUCTIONS
|
|
1
|
Select Catalog from the menu located on the upper left corner of the Custom Learning Center screen.
|
|
2
|
Use the catalog filter and select Interactive Care Reviewer-Online Authorizations or Authorizations from the Category menu.
|
|
3
|
Click Apply and then enroll for the courses (videos) you want to view.
|
Illustrated reference guides that you can print are located on Custom Learning Center Resources. Select Resources from the menu located on the upper left corner of the screen. Use the catalog filter and select Authorizations or Interactive Care Reviewer-Online Authorizations from the Category menu. Select Download to view and/or print the reference guide.
640-0920-PN-VA
UPDATE: We are offering providers who are using Change Healthcare for revenue cycle management an opportunity to have a streamlined in-workflow solution native to Relay Assurance application.
Starting September 1, 2020, Anthem Blue Cross and Blue Shield will launch the use of Change Healthcare’s Medical Attachment functionality for electronic communications as an additional digital option. This new functionality allows providers to upload medical records and itemized bill documents electronically instead of through traditional paper communications. This functionality can improve communications and increase transparency for medical record requests and will not otherwise impact the audit program.
Important facts regarding this change:
- This change only affects providers who use Assurance Reimbursement Management™ from Change Healthcare and have opted in to using the Attach Assist functionality.
- The new functionality is only for medical record requests for postpay claims for the Payment Integrity Quality Claims Review (Provider Audit) department only.
- There will be no duplicate requests (either paper or electronic). If you opt to use this method, paper requests for medical records will not be sent.
- In Assurance Reimbursement Management™, requests for additional documentation will be displayed to the user on the History tab of the claim. Assurance will be configured such that these requests drive workflow to ensure they are brought to the user’s attention.
|
The original letter, historically sent via paper, is accessible as a PDF electronic copy in the provider’s downloads folder in Assurance for review. The letter content is exactly the same as it was in paper format.
|
|
Each request letter (first, second and final attempt) will have a time frame for responding to the request. After the time frame has passed for that letter, you will not be able to respond to that letter. If you wish to upload medical records after the response time has expired, please refer to the Change Healthcare training referenced below.
|
|
Providers can respond to the request by uploading records in Assurance Attach Assist. The attachments are received in almost real time and are delivered electronically to the payer’s systems through secure means. Records can be accessed through a hyperlink in Assurance Attach Assist for the particular claim the record is associated.
|
- The following is out of scope or not impacted:
|
Vendor requests for medical records on behalf of the payer.
|
|
Providers who do not use Assurance Reimbursement Management™ Attach Assist from Change Healthcare or have not configured Attach Assist within Assurance Reimbursement Management.™
|
|
The request timing of request letter and the verbiage in the request letter.
|
|
The Program Integrity Special Investigations Unit postpay review is not included at this time.
|
Resources
Training is available on the Change Healthcare Connect Center at:
https://rcmknowledgecenter.changehealthcare.com/learn
Can I start using the functionality earlier?
Yes, you can. If you chose to opt in earlier, please ensure you are configured within Assurance Reimbursement Management™. Reach out to your Provider Solutions contact or request early access via email at dl-Prod-ChangeHealthcare-Provider-Support@anthem.com.
For additional information, see our Change Healthcare Medical Attachment Functionality FAQ to the right under the "Article Attachments" section.
617-0920-PN-VA
On November 12, 2020, Anthem will offer our final provider education webinar for the year. Register today to secure your place for the session. Designed for our network-participating providers, the webinar addresses Anthem business updates and billing guidelines that impact your business interactions with us.
For your convenience, we offer these informative, hour-long sessions online to eliminate travel time and help minimize disruptions to your office or practice. The date for the fall webinar is:
- Thursday, November 12, 2020: 11 a.m. to Noon ET
Please take time to register now for the webinar using the registration form to the right under the “Article Attachments” section. If you have already registered for the November webinar, please ensure you have received a confirmation from an Anthem representative noting we’ve received your registration form. Contact joyce.lindley@anthem.com if you need to confirm your registration.
607-0920-PN-VA Claims that are submitted for laboratory services subject to the Clinical Laboratory Improvement Amendments (CLIA) 1988 federal statute and regulations require additional information to be considered for payment.
A valid CLIA certificate identification number is required for reimbursement of clinical laboratory services reported on a CMS-1500 claim form (or its electronic equivalent) beginning October 1, 2020. The CLIA certificate identification number must be submitted in one of the following ways:
|
Claim Format and Elements
|
CLIA Number Location Options
|
Referring Provider Name and National Provider Identifier (NPI) Number Location Options
|
|
CMS-1500
|
Must be represented in field 23
|
Submit the referring provider name and NPI number in fields 17 and 17b, respectively.
|
|
Electronic transaction 837 Professional; Health Insurance Portability and Accountability Act (HIPAA) Version 5010
|
Must be represented in the 2300 loop, REF02 element, with qualifier of “X4” in REF01
|
Submit the referring provider name and NPI number in the 2310A loop, NM1 segment.
|
Providers who have obtained a CLIA Waiver or Provider Performed Microscopy Procedure accreditation must include the “QW” modifier when any CLIA waived laboratory service is reported on a CMS-1500 claim form in order for the procedure to be evaluated to determine eligibility for benefit coverage.
Laboratory procedures are only covered and therefore payable if rendered by an appropriately licensed or certified laboratory. Therefore, any claim that does not contain the CLIA ID will be considered incomplete and rejected beginning October 1, 2020.
If you have additional questions, please call the telephone number on the back of the member’s identification card.
614-0920-PN-VA Anthem’s collaborative business relationships with oncology practices, which include sharing of relevant data, have helped drive improved outcomes. Our “Potentially Avoidable Admissions During Chemo” model uses predictive analytics to equip oncologists with actionable, patient-level data to highlight those at greatest risk for complications during chemotherapy.
Since the launch of this model, early results indicate success, as observed by a 13% reduction in avoidable inpatient admissions.1
Our oncology partners have recognized the value of this predictive modeling capability and routinely supplement their own information to proactively outreach to patients who may benefit from additional support during treatment.
Mary Scott, RN, from City of Hope* says this data enables them make better decisions about patient care, “…best part [of this model] is having some data and some information and some specifics about patients that are deemed to be at risk and keeping them out of the hospital, which is a pretty critical part of our work. I think with the Anthem information we've been able to tackle that in a much better and more organized fashion because they provide us with a list of patients that are high risk, medium risk, and low risk for admission, people who are on chemotherapy, and these regimens can be pretty complicated, pretty toxic, and it helps us to make those better decisions for their care.”
Watch this video to hear more about how our collaborative partnerships with oncology practices is leading to improved outcomes.
For more information on Anthem’s Cancer Care Solutions, email cancer.quality@anthem.com or contact your Anthem Oncology Provider Clinical Liaison.
*City of Hope continues to conduct innovative research to advance programs targeted at eliminating cancer, diabetes and other serious chronic illnesses.
1 Anthem internal data. Among providers who participate in Anthem’s Cancer Care Solutions programs we observed 12.8% fewer avoidable inpatient days per 1,000 over baseline. Based on Anthem commercial business, January through December 2019.
626-0920-PN-VA
As a provider, you are committed to providing the best care for our members, which may now include telehealth visits. Telehealth visits are an acceptable form for seeing your patients, and assessing if they have risk adjustable conditions in support of the Anthem Commercial Risk Adjustment (CRA) prospective program.
The prospective program is well under way for 2020, and focuses on member health assessments for patients with undocumented Hierarchical Condition Categories (HCCs), in order to help close patients’ gaps in care. We continue to provide updates regarding the prospective program to solicit your help getting patients in for a wellness visit before the calendar year ends, and we offer incentives to recognize your efforts (see details below.)
Inovalon requests
Inovalon – an independent company that provides secure, clinical documentation services – helps us comply with the provisions of the Affordable Care Act (ACA) that require us to assess members’ relative health risk levels. Please submit health assessments to Inovalon when completed and if you have questions, you can reach Inovalon directly at 1-877-448-8125.
Prospective program ask of providers:
Anthem network providers – usually primary care providers (PCPs) – receive letters from Inovalon, requesting that they:
- Schedule a comprehensive in person or telehealth visit with patients identified by Inovalon to confirm or deny if previously coded or suspected diagnoses exists, and;
- Submit a Health Assessment documenting the previously coded or suspected diagnoses (also called SOAP Notes - Subjective, Objective, Assessment and Plan).
Incentives offered for properly submitted Health Assessments:
- $100 for each Health Assessment properly submitted electronically via Inovalon’s ePASS® tool
- $50 for each Health Assessment properly submitted via fax
ePASS training is available to ensure health assessment completion accuracy:
- Training webinars every Wednesday, 3 – 4 p.m. EST.
- Register by sending an email to ePASSProviderRelations@inovalon.com with your name, organization, contact information and the date of the webinar you wish to attend. Information will be provided on how to join the webinar.
Alternative engagement
Inovalon’s ePASS® tool is our preferred method for submission. However, we offer alternate options to be flexible and meet your needs. If in 2019 your practice utilized these alternative options for prospective member outreach, we thank you for continuing to utilize these alternative forms of program participation in 2020.
For those providers not familiar with alternative options, they are listed here. Telehealth visits are also an acceptable form of a patient visit for these alternative engagement options. Any questions can be directed to either your local Provider Representative, or the Anthem CRA network education representative listed below.
- EPHC Providers using PCMS - Providers participating in our Enhanced Personal Health Care (EPHC) program can use member reports from our PCMS tool to schedule members for comprehensive visits. PCMS does have a link to take you directly to the Inovalon ePASS® tool where completed health assessments will result in a $100 incentive payment per submitted health assessment.
- List of Members to be scheduled - Anthem CRA provides member/patient reports for providers to schedule members for comprehensive visits. No health assessment needed. Not eligible for additional incentive because CRA will get the diagnosis for gap closure through claims submission.
- EPIC Patient Assessment Form (PAF) - Providers with EPIC as their electronic medical record (EMR) system can fax the EPIC PAF to Anthem CRA at 1-855-244-0926 with a coversheet indicating "see attached Anthem Progress Note,” which is eligible for a $50 incentive payment.
- Providers Existing Patient Assessment Form (PAF) - Utilizes providers’ existing EMR system and applicable PAF. Must be submitted to Anthem CRA at 1-855-244-0926 with coversheet indicating, "see attached Anthem Progress Note,“ which is eligible for a $50 incentive payment.
If you have questions, please contact Commercial Risk Adjustment network education representative – Alicia.Estrada@anthem.com.
Thank you for your commitment to assessing your patients’ health and closing possible gaps in care.
623-0920-PN-VA
Effective with dates of service on and after October 1, 2020, and in accordance with the IngenioRx Pharmacy and Therapeutics (P&T) process, Anthem Blue Cross and Blue Shield will update our drug lists that support Commercial health plans. Updates include changes to drug tiers and the removal of medications from the formulary.
As certain brand and generic drugs will no longer be covered, providers are encouraged to determine if a covered alternative drug is appropriate for their patients whose current medication will no longer be covered. Communications to providers and their patients affected by the changes went out in early August.
Please note, this update does not apply to the Select Drug List and does not impact Medicaid and Medicare plans. To ensure a smooth member transition and minimize costs, providers should review these changes and consider prescribing a drug on formulary or on a lower tier, if appropriate.
View a summary of changes.
634-0920-PN-VA Prior authorization updates
Effective for dates of service on and after December 1, 2020, the following specialty pharmacy codes from current or new clinical criteria documents will be included in our prior authorization review process.
Please note, inclusion of NDC code on your claim will help expedite claim processing of drugs billed with a Not Otherwise Classified (NOC) code.
Access the clinical criteria information.
For Anthem Blue Cross and Blue Shield and our affiliate HealthKeepers, Inc., prior authorization clinical review of these specialty pharmacy drugs will be managed by Anthem. Drugs used for the treatment of Oncology will still require pre-service clinical review by AIM Specialty Health® (AIM), a separate company.
This applies to members with Preferred Provider Organization (PPO), HealthKeepers (HMO), POS AdvantageOne, and Act Wise (CDH plans).
|
Clinical Criteria
|
HCPCS or CPT Code(s)
|
Drug
|
|
ING-CC-0164
|
J3490
J9999
C9399
|
Jelmyto
|
|
ING-CC-0165
|
J3490
J3590
J9999
C9399
|
Trodelvy
|
|
ING-CC-0061
|
J1950
J3490
|
Fensolvi
|
*Non oncology use is managed by Anthem’s medical specialty drug review team. Oncology use is managed by AIM.
Site of care updates
Effective for dates of service on and after December 1, 2020, the following specialty pharmacy codes from current or new clinical criteria documents will be included in our existing prior authorization site of care review process.
Access the site of care drug list.
For Anthem Blue Cross and Blue Shield and affiliate HealthKeepers, Inc., prior authorization clinical review of these specialty pharmacy drugs will be managed by Anthem. Drugs used for the treatment of Oncology will still require pre-service clinical review by AIM Specialty Health® (AIM), a separate company.
This applies to members with Preferred Provider Organization (PPO), HealthKeepers (HMO), POS AdvantageOne, and Act Wise (CDH plans).
|
Clinical Criteria
|
HCPCS or CPT Code(s)
|
Drug
|
|
ING-CC-0153
|
J0791
|
Adakveo (crizanlizumab)
|
|
ING-CC-0139
|
J3111
|
Evenity (romosozumab)
|
|
ING-CC-0154
|
J0223
|
Givlaari (givosiran)
|
|
ING-CC-0156
|
J0896
|
Reblozyl (luspatercept)
|
|
ING-CC-0003
|
J1558
|
Xembify (immune globulin)
|
|
*ING-CC-0002
|
Q5120
|
Ziextenzo (pegfilgrastim-bmez)
|
*Non oncology use is managed by Anthem’s medical specialty drug review team. Oncology use is managed by AIM.
REMINDER: Process for Medical Non-Oncology Specialty Drug reviews
Please follow these steps to submit medical non-oncology specialty drug reviews:
|
Action
|
Contact
|
|
Submit a new prior authorization request for a medical specialty drug review
Submit a re-authorization request for a medical specialty drug review previously performed by AIM
|
Call IngenioRx at 1-833-293-0659
or
Fax IngenioRx at 1-888-223-0550
|
|
Inquire about an existing request (initially submitted to AIM or IngenioRx), peer-to-peer review, or reconsideration
|
Call IngenioRx
|
Please note:
- AIM continues to be responsible for performing medical oncology drug reviews for existing commercial medical benefit for our employer group business.
- Post-service clinical coverage reviews and grievance and appeals process and teams have not changed.
637-0920-PN-VAState & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 Discharge planningDischarge planning is the process of identifying and preparing for a patient’s anticipated health care needs after they have transitioned from the hospital to home. It is a process that involves the engagement of the Anthem HealthKeepers Plus member (your patient), family, and health care team. If done correctly, effective discharge planning improves patient safety, patient quality and cost outcomes.
Statistical data
Health disparities are known to contribute to readmission risks. Medicaid readmissions are considered significant; therefore, they can be widespread and costly. Statistical data is shown below:
- Medicaid all-cause 30-day readmission rates for patients ages 21 to 44 (19.2%) and 45 to 64 (21.6%) are higher than Medicare readmission rates (17.3%).
- Nearly 20% of members experience an adverse event within three weeks of discharge.
- Three quarters of adverse events could have been prevented with proper discharge planning.
- The most common complications post-discharge include adverse drug events, hospital acquired infections and procedural complications.
- Nearly 20% of Medicare patients were re-hospitalized within 30 days after discharge.
- Approximately 70% of surgical patients were re-hospitalized with a medical problem.
- The cost of unplanned hospitalization in 2004 was $17.4 billion.
Background
Under the Affordable Care Act, there are certain hospital readmissions that could lead to a penalty and cause lower reimbursements. In 2012, there were more than 2,000 hospitals penalized related to preventable readmissions. This specific mandate has caused the need to focus in on patient-centered care and a discharge plan that is all-inclusive. Discharge planning can be a complex process; however, having safe transitions from the hospital to home is a top priority. The IDEAL discharge planning strategy seeks to engage the patient and family in the discharge planning process. Building effective relationships with the member and family will ensure patient quality and patient safety. Embracing a culture of open communication will optimally lead to positive patient outcomes and help to make the transition to home safe and effective.
The IDEAL Discharge Planning strategy
There are many ways to promote effective discharge planning. This article focuses on the IDEAL Discharge Planning Strategy. The IDEAL Discharge Planning strategy is a strategic way to engage the patient and family in the discharge planning process. Its focus is on a culture of inclusivity:
- Include the patient and the family in the complete discharge planning process. This is a process that carries on throughout the entire hospitalization. Determine who will provide care for the patient at home and be sure to include this individual in the team meetings and conversations.
- Discuss with the patient and family five areas to prevent problems when they return home. These five areas include home life, medication reconciliation, potential warning signs and concerns, test results with thorough instructions, and follow-up appointments with providers.
- Educate the patient and family in layman terms about his/her condition and the discharge process. Complete education throughout the entire hospital stay. Address patient and family goals at admission and throughout the hospital stay.
- Assess how well the information has been provided to the patient by the doctors, nurses and other health care professionals and use the teach-back method to ensure understanding. Avoid overloading the member with too much information.
- Listen to and respect the patient and family’s goals, preferences, observations and concerns. Use motivational interviewing such as open-ended questions to spark questions and concerns. Schedule a meeting prior to discharge with patient, family, and interdisciplinary team.
Challenges to discharge planning:
- Fragmented care due to multiple providers and inability to keep scheduled appointments.
- Medication reconciliation discrepancy (complex or high-risk medications).
- Inadequate discharge preparation.
- Miscommunication between provider, patient and family.
- Communication and education not properly completed.
- Information or educational offerings not provided in layman terms.
- Appropriate teachings based on how the patient best learns not utilized (verbal, audiovisual).
- Inability to have patient self-manage his/her condition.
Evidence-based practices to improve discharge planning:
- Come up with your own discharge planning sheets or checklists and follow them per your facility policies and procedures.
- Provide trainings on effective discharge planning with nursing staff and allow staff to feel a part of the process.
- Empower patients through educational activities throughout the stay to help them better understand their conditions, manage their diet, manage activities, manage medications, manage care regimens and manage follow-up care.
- Provide attention to discharge planning on the first day of admission and throughout the entire stay, providing a multidisciplinary approach.
- Develop a plan for care coordination after discharge and complete any follow-up appointments prior to the patient leaving the facility.
- Always implement practices or set aims to improve discharge planning in your facility.
References
Agency for Healthcare Research and Quality (2017, December). Strategy 4: Care transitions
from hospital to home: IDEAL discharge planning. Retrieved from https://www.ahrq.gov/professionals/systems/hospital/engagingfamilies/strategy4/index.html
Barrett, M.L., Weir, L.M., Jiang J. H., Steiner, C.A. (2015). Cup statistical brief #199: All-cause readmissions by payer and age, 2009–2013. AHRQ Healthcare Cost and Utilization Project. Retrieved from http://www.hcup-us.ahrq.gov/reports/statbriefs/sb199-Readmissions-Payer-Age.pdf. Accessed April 13, 2020.
Torrey, T. (2020). Discharges and readmissions. Verywell health. Information about ACA
Hospital Discharges and Readmissions. Retrieved from https://www.verywellhealth.com/affordable-care-act-hospitals-2614805
AVA-NU-0264-20State & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 CLIA Certificate of WaiverThis information pertains to Anthem HealthKeepers Plus providers.
Effective October 1, 2019, HealthKeepers, Inc. implemented the edits for Clinical Laboratory Improvement Amendments of 1988 (CLIA).
As a reminder, if you were issued a Certificate of Waiver type of CLIA Certificate, you can only perform specific waived tests.
If you are unsure of what your certificate level is, please refer to the Laboratory Demographics Lookup at https://tinyurl.com/Laboratory-Demographics-Lookup.
The CLIA number needs to be included on the claim. In addition, the service address must match the address of record noted on the CMS Provider of Service File.
If you receive a GLI denial, it means that the CLIA number is missing on the claim, or your service address is not matching the address on file with CMS. The first three characters of the address in CMS are compared with the billing and servicing address on the claim to try to make a match. This is to ensure that each location is registered with their own CLIA number.
If you receive a GLJ denial, it indicates that the level of certification of the CLIA submitted on the claim is not a high enough level for the procedure being billed.
Please refer to the below links for additional information regarding CLIA edits.
List of waived tests:
https://tinyurl.com/categorization-of-tests
General information and FAQ:
https://tinyurl.com/CLIA-FAQ
How to obtain a CLIA Certificate:
https://tinyurl.com/CLIA-Certificate
If you have any questions about this communication, call Provider Services at 1‑800‑901‑0020 or Anthem CCC Plus Provider Services at 1‑855‑323‑4687.
AVA-NU-0267-20State & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 What Matters Most online training course: Improving patient experienceThe What Matters Most online training course for Anthem HealthKeepers Plus network providers and office staff addresses gaps in care and offers approaches to communication with patients. The course is available at no cost and is eligible for one CME credit by the American Academy of Family Physicians. The What Matters Most online training course can be accessed at: www.patientexptraining.com.
If you have any questions about this communication, call Provider Services at 1‑800‑901‑0020 or Anthem CCC Plus Provider Services at 1‑855‑323‑4687.
AVA-NU-0272-20
State & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 Medical drug benefit Clinical Criteria updatesOn May 15, 2020, the Pharmacy and Therapeutics (P&T) Committee approved Clinical Criteria applicable to the Anthem HealthKeepers Plus medical drug benefit for HealthKeepers, Inc. These policies were developed, revised or reviewed to support clinical coding edits.
The Clinical Criteria is publicly available on the provider websites, and the effective dates will be reflected in the Clinical Criteria Web Posting May 2020. Visit Clinical Criteria to search for specific policies.
If you have questions or would like additional information, use this email.
AVA-NU-0273-20State & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 Coverage Guidelines and Clinical Utilization Management Guidelines updateThe Coverage Guidelines, Clinical Utilization Management (UM) Guidelines and Third Party Criteria below, which are applicable to Anthem HealthKeepers Plus members, were developed and/or revised to support clinical coding edits. Note, several policies and guidelines were revised to provide clarification only and are not included. Existing precertification requirements have not changed.
Please share this notice with other members of your practice and office staff.
To view a guideline, visit https://www11.anthem.com/search.html.
Notes/updates:
Updates marked with an asterisk (*) notate that the criteria may be perceived as more restrictive.
- CG-DME-46 — Pneumatic Compression Devices for Prevention of Deep Vein Thrombosis of the Extremities in the Home Setting
|
Expanded scope of document and revised Medically Necessary statement
|
- CG-DME-47 — Noninvasive Home Ventilator Therapy for Respiratory Failure
|
Revised Medically Necessary and Discussion/General Information sections
|
- CG-GENE-02 — Analysis of RAS Status
|
Clarified scope of document and revised the Not Medically Necessary and Coding sections
|
- CG-MED-64 — Transcatheter Ablation of Arrhythmogenic Foci in the Pulmonary Veins as a Treatment of Atrial Fibrillation or Atrial Flutter (Radiofrequency and Cryoablation)
|
Revised the Medically Necessary statement
|
- CG-MED-68 — Therapeutic Apheresis
|
Revised Medically Necessary, Not Medically Necessary, Coding and Discussion/General Information sections
|
- DME.00011 — Electrical Stimulation as a Treatment for Pain and Other Conditions: Surface and Percutaneous Devices
|
Revised Investigational and Not Medically Necessary, Rationale and Coding sections
|
- MED.00004 — Technologies for the Evaluation of Skin Lesions (including Dermatoscopy, Epiluminescence Microscopy, Videomicroscopy, Ultrasonography)
|
Revised the Not Medically Necessary, Rationale and Coding sections
|
Coverage Guidelines
On November 7, 2019, February 20, 2020, and May 14, 2020, the Medical Policy and Technology Assessment Committee (MPTAC) approved the following Coverage Guidelines applicable to Anthem HealthKeepers Plus members.
|
Publish date
|
Coverage Guidelines number
|
Coverage Guidelines title
|
New or revised
|
|
7/8/2020
|
*DME.00042
|
Electronic Positional Devices for the Treatment of Obstructive Sleep Apnea
|
New
|
|
7/8/2020
|
*MED.00131
|
Electronic Home Visual Field Monitoring
|
New
|
|
7/1/2020
|
*MED.00132
|
Adipose-derived Regenerative Cell Therapy and Soft Tissue Augmentation Procedures
|
New
|
|
7/8/2020
|
*MED.00133
|
Ingestion Event Monitors
|
New
|
|
7/8/2020
|
*THER-RAD.00012
|
Electrophysiology-Guided Noninvasive Stereotactic Cardiac Radioablation
|
New
|
|
2/5/2020
|
*GENE.00052
|
Whole Genome Sequencing, Whole Exome Sequencing, Gene Panels, and Molecular Profiling
|
New
|
|
4/15/2020
|
*DME.00041
|
Low Intensity Therapeutic Ultrasound for the Treatment of Pain
|
New
|
|
4/15/2020
|
*GENE.00053
|
Metagenomic Sequencing for Infectious Disease in the Outpatient Setting
|
New
|
|
4/15/2020
|
*GENE.00054
|
Paired DNA and Messenger RNA (mRNA) Genetic Testing to Detect, Diagnose and Manage Cancer
|
New
|
|
4/15/2020
|
*SURG.00154
|
Microsurgical Procedures for the Treatment of Lymphedema
|
New
|
|
2/27/2020
|
*SURG.00155
|
Cryoneurolysis for Treatment of Peripheral Nerve Pain
|
New
|
|
5/21/2020
|
DME.00009
|
Vacuum Assisted Wound Therapy in the Outpatient Setting
|
Revised
|
|
7/8/2020
|
*DME.00011
|
Electrical Stimulation as a Treatment for Pain and Other Conditions: Surface and Percutaneous Devices
|
Revised
|
|
5/21/2020
|
DME.00034
|
Standing Frames
|
Revised
|
|
7/8/2020
|
*MED.00004
|
Technologies for the Evaluation of Skin Lesions (including Dermatoscopy, Epiluminescence Microscopy, Videomicroscopy, Ultrasonography)
|
Revised
|
|
5/21/2020
|
SURG.00026
|
Deep Brain, Cortical, and Cerebellar Stimulation
|
Revised
|
|
5/21/2020
|
SURG.00047
|
Transendoscopic Therapy for Gastroesophageal Reflux Disease, Dysphagia and Gastroparesis
|
Revised
|
Clinical UM Guidelines
On November 7, 2019, February 20, 2020 and May 14, 2020, the MPTAC approved the following Clinical UM Guidelines applicable to Anthem HealthKeepers Plus members. These guidelines were adopted by the medical operations committee for Anthem HealthKeepers Plus members on November 28, 2019, April 23, 2020 and May 25, 2020.
|
Publish date
|
Clinical UM Guideline number
|
Clinical UM Guideline title
|
New or revised
|
|
4/15/2020
|
*CG-ANC-08
|
Mobile Device-Based Health Management Applications
|
New
|
|
7/1/2020
|
*CG-SURG-107
|
Surgical and Minimally Invasive Treatments for Benign Prostatic Hyperplasia (BPH)
|
New
|
|
4/15/2020
|
*CG-SURG-108
|
Stereotactic Radiofrequency Pallidotomy
|
New
|
|
7/8/2020
|
*CG-DME-46
|
Pneumatic Compression Devices for Prevention of Deep Vein Thrombosis of the Extremities in the Home Setting
|
Revised
|
|
7/8/2020
|
*CG-DME-47
|
Noninvasive Home Ventilator Therapy for Respiratory Failure
|
Revised
|
|
7/8/2020
|
*CG-GENE-02
|
Analysis of RAS Status
|
Revised
|
|
5/21/2020
|
CG-MED-44
|
Holter Monitors
|
Revised
|
|
7/8/2020
|
*CG-MED-64
|
Transcatheter Ablation of Arrhythmogenic Foci in the Pulmonary Veins as a Treatment of Atrial Fibrillation or Atrial Flutter (Radiofrequency and Cryoablation)
|
Revised
|
|
7/8/2020
|
*CG-MED-68
|
Therapeutic Apheresis
|
Revised
|
|
5/21/2020
|
CG-MED-74
|
Implantable Ambulatory Event Monitors and Mobile Cardiac Telemetry
|
Revised
|
|
5/21/2020
|
CG-MED-77
|
SPECT/CT Fusion Imaging
|
Revised
|
|
5/21/2020
|
CG-SURG-27
|
Gender Reassignment Surgery
|
Revised
|
|
5/21/2020
|
CG-SURG-98
|
Prostate Biopsy using MRI Fusion Techniques
|
Revised
|
AVA-NU-0276-20 State & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 Quarterly pharmacy formulary change noticeThe formulary changes listed in the table below apply to all Anthem HealthKeepers Plus members (including those enrolled in FAMIS [the CHIP program] and Medallion [the Medicaid program]) and Anthem HealthKeepers Plus, Commonwealth Coordinated Care Plus (Anthem CCC Plus) members. These changes were reviewed and approved at the fourth quarter pharmacy and therapeutics committee meeting.
Effective August 1, 2020, formulary changes, non-formulary changes and prior authorization (PA) requirements will apply. Remember to read the footnotes at the end of the table.
|
Effective for all members on August 1, 2020
|
|
Therapeutic class
|
Medication
|
Formulary status change
|
Potential alternatives
(preferred products)
|
|
Continuous Blood Glucose System
|
DEXCOM GLUCOSE AND
FREESTYLE LIBRE SYSTEM
SENSOR
TRANSMITTER
RECEIVER
|
Preferred with PA under the pharmacy benefit
|
n/A
|
|
Edits effective August 1, 2020
No changes in preferred/nonpreferred status revision or addition to UM edit only
|
|
Therapeutic class
|
Medication
|
Formulary status change
|
|
ACNE PRODUCTS
|
AKLIEF CRE 0.005%
|
ADD PA
ADD QL
1 pump per 30 days
|
|
AMZEEQ AER 4%
|
ADD PA
ADD QL
30 GRAMS PER 30 DAYS
|
|
ABSORICA LD CAP 8MG
ABSORICA LD CAP 16MG
ABSORICA LD CAP 24MG
ABSORICA LD CAP 32MG
|
ADD PA
add ql
30 day supply per fill
|
|
ADENOSINE TRIPHOSPHATE-CITRATE LYASE (ACL) INHIBITORS
|
NEXLETOL TAB 180MG
|
ADD PA
ADD QL
1 TABLET PER DAY
|
|
AGENTS FOR CONSTIPATION
|
IBSRELA TAB 50 MG*
|
add pa
add ql
2 TABLETS per day
|
|
AGENTS FOR CONSTIPATION
|
PIZENSY*
|
add pa; add ql
20 grams per day
|
|
ALS AGENTS
|
EXSERVAN 50 MG FILM*
|
add st
add pa
add ql
4 films per day
|
|
ANTICONVULSANTS - BENZODIAZEPINES
|
VALTOCO SPR 5MG
|
ADD PA
ADD QL
10 CARTONS PER 30 DAYS
|
|
ANTIDIABETIC COMBINATIONS
|
TRIJARDY XR TAB 5-2.5-1000MG
TRIJARDY XR TAB 12.5-2.5-1000MG
|
ADD ST
ADD QL
2 TABLETS PER DAY
|
|
TRIJARDY XR TAB 10-5-1000MG
TRIJARDY XR TAB 25-5-1000MG
|
ADD ST
ADD QL
1 TABLET PER DAY
|
|
ANTIHYPERLIPIDEMICS
|
NEXLIZET TAB 180MG*
|
add pa
Add ql
1 tablet per day
|
|
ANTIMETABOLITES
|
REDITREX INJ*
|
add pa
add ql
4 auto-injectors per 28 days
|
|
ANTINEOPLASTIC - ANTIBODIES
|
PADCEV INJ 20MG
ENHERTU INJ 100MG
|
add pa
|
|
ANTINEOPLASTIC ENZYME INHIBITORS
|
AYVAKIT TAB 100MG
|
ADD PA
ADD QL
1 tablet per day
|
|
TAZVERIK TAB 200MG
|
ADD PA
ADD QL
8 tablets per day
|
|
ATTENTION-DEFICIT/HYPERACTIVITY DISORDER (ADHD) AGENTS
|
KAPVAY TAB 0.1 MG
|
ADD QL
4 tablets per DAY
|
|
BONE DENSITY REGULATORS
|
BONSITY INJ 620MCG/2.48ML*
|
add pa
add ql
1 pen per 28 days
|
|
CALCITONIN GENE-RELATED PEPTIDE (CGRP) RECEPTOR ANTAG
|
VYEPTI INJ 100MG/ML
|
add pa
ADD ST
ADD QL
1 vial per 3 months
|
|
NURTEC CHW 75MG ODT
|
ADD ST
ADD QL
15 tablets per 30 days
|
|
DIBENZAPINES
|
SECUADO DIS 3.8MG
|
ADD QL
1 patch per day
|
|
FERTILITY REGULATORS
|
NOVAREL INJ 5000UNIT
NOVAREL INJ 10000UNIT
PREGNYL INJ 10000UNT
OVIDREL INJ
|
add pa
|
|
GLUCOCORTICOSTEROIDS
|
HEMADY TAB 20MG*
|
add pa
add ql
2 tablets per day
|
|
HEMATOPOIETIC GROWTH FACTORS
|
ZIEXTENZO INJ 6/0.6ML
|
add pa
add ql
2 syringes
|
|
REBLOZYL INJ 25MG
REBLOZYL INJ 75MG
|
add pa
|
|
UDENYCA INJ 6MG/.6ML
|
add st
add pa
|
|
NEULASTA INJ 6MG/0.6M
FULPHILA INJ 6/0.6ML
|
add pa
|
|
OTIC COMBINATIONS
|
CORTISPORIN SUS -TC OTIC
|
add st
|
|
PLEUROMUTILINS
|
XENLETA TAB 600MG
|
add pa
add ql
10 tablets per fill;
1 fill per 30 days
|
|
PROTECTIVES AGAINST UV RADIATION
|
SCENESSE IMP 16MG
|
add pa
add ql
1 implant per 2 months
|
|
SOMATOSTATIC AGENTS
|
BYNFEZIA PEN 2500MCG/ML
|
add pa
add ql
1 pen per 14 days
|
|
TARGETED IMMUNE MODULATORS
|
AVSOLA 100MG VIAL*
|
add pa
|
|
ABRILADA 10 MG/0.2 ML, 20 MG/0.4 ML PREFILLED SYRINGE
|
add pa
add ql
2 pens/syringes per 28 days
|
|
ABRILADA 40MG/0.8 ML PREFILLED PEN/SYRINGE
|
add pa
add ql
2 syringes per 28 days
|
* Medication will be added to the formulary when it is available on the market.
What action do I need to take?
Please review these changes and work with your Anthem HealthKeepers Plus patients and/or Anthem CCC Plus patients to transition them to formulary alternatives. If you determine formulary alternatives are not clinically appropriate for specific patients, you will need to obtain PA to continue coverage beyond the applicable effective date.
What if I need assistance?
We recognize the unique aspects of patient cases. If your patients cannot be converted to a formulary alternative, call our Pharmacy department at 1-800-901-0020 (Anthem HealthKeepers Plus members) or 1-855-323-4687 (Anthem CCC Plus members) and follow the voice prompts for pharmacy PA. You can find the Preferred Drug List (formulary) on our provider website at https://mediproviders.anthem.com/va > Pharmacy > Medicaid Common Core Formulary > Common Core Preferred Drug List.
If you have any questions about this communication, call Provider Services at 1‑800‑901‑0020 or Anthem CCC Plus Provider Services at 1‑855‑323‑4687.
AVA-NU-0279State & Federal | HealthKeepers, Inc. | Anthem HealthKeepers Plus Medicaid products | September 1, 2020 Keep up with Medicaid newsOn May 15, 2020, the Pharmacy and Therapeutics (P&T) Committee approved Clinical Criteria applicable to the medical drug benefit for Anthem Blue Cross and Blue Shield. These policies were developed, revised or reviewed to support clinical coding edits.
The Clinical Criteria is publicly available on the provider websites, and the effective dates will be reflected in the Clinical Criteria Web Posting May 2020. Visit Clinical Criteria to search for specific policies.
If you have questions or would like additional information, use this email.
ABSCRNU-0162-20 511673MUPENMUB AIM Specialty Health® (AIM)* administers the musculoskeletal program for Medicare Advantage members, which includes the medical necessity review of certain surgeries of the spine, joints and interventional pain treatment. For certain surgeries, the review also includes a consideration of the level of care.
Effective December 1, 2020, two joint codes (29871 and 29892) will be incorporated into the AIM Level of Care Guideline for Musculoskeletal Surgery and Procedures. According to the clinical criteria for level of care, which is based on clinical evidence as outlined in the AIM guideline, it is generally appropriate to perform these two procedures in a hospital outpatient setting. To avoid additional clinical review for these surgeries, providers requesting prior authorization should either choose hospital observation admission as the site of service or Hospital Outpatient Department (HOPD).
We will review requests for inpatient admission and will require the provider to substantiate the medical necessity of the inpatient setting with proper medical documentation that demonstrates one of the following:
- Current postoperative care requirements are of such an intensity and/or duration that they cannot be met in an observation or outpatient surgical setting.
- Anticipated postoperative care requirements cannot be met, even initially, in an observational surgical setting due to the complexity, duration, or extent of the planned procedure and/or substantial preoperative patient risk.
On January 1, 2020, CMS removed total hip arthroplasty as well as six spine codes from the inpatient only (IPO) list, making these procedures eligible for payment by Medicare in the hospital outpatient setting in addition to the hospital inpatient setting. The two-midnight rule should guide providers on the expected reimbursement. The codes that were removed from the inpatient only list and are also in the AIM Musculoskeletal program are 27130, 22633, 22634, 63265 and 63267. CMS has established a two year grace period (ending December 31, 2021) for site of service reviews of these codes in order to facilitate provider transition to compliance with the two-midnight rule.
To this end, it is recommended that providers choose hospital observation or Hospital Outpatient Department (HOPD) during the prior authorization process when clinically appropriate to the respective patient. Choosing hospital observation still allows for the surgery to be performed and recovered in the main hospital, so long as discharge is planned for less than two midnights. Alternatively, the provider may choose to perform the procedure in the Hospital Outpatient Department (HOPD). However, the inpatient setting will still be approved should the provider decide it is the optimal setting for the member.
Providers should continue to submit prior authorization requests to AIM using one of the following ways:
- Access AIM ProviderPortalSM directly at http://providerportal.com. Online access is available 24/7 to process orders in real-time, and is the fastest and most convenient way to request authorization.
- Call the AIM toll-free number at 1-800-714-0400, Monday through Friday 8 a.m. to 8 p.m. ET.
If you have questions, please contact the provider number on the back of the member’s ID card.
ABSCRNU-0163-20 511827MUPENMUB |