Provider News NevadaJuly 1, 2021 July 2021 Anthem Provider News - NevadaIt wasn’t too long ago when patients taking warfarin (brand name Coumadin) were heading off to the lab or clinic every few weeks for an international normalized ratio (INR) blood test. Thanks to a small, portable device, patients on warfarin can now self-test with a finger prick drop of blood. There is more to self-testing than the ease and convenience, though. Patients are happier! Their quality of life improved because they can keep up with their activities – even travel, without the stress of making and keeping testing appointments.
Self-testing: Measurable difference when correct coding is reflected
This type of quality care and improved outcomes are making a measurable difference in the lives of our members. We want this success accounted for in the INR clinical quality measure and with your help, we can do it. Use these codes to reflect INR In-home monitoring when noting the INR results for your patients.
|
Value set ID and subgroup
|
Code
|
Description
|
|
INR HOME MONITORING
|
CPT CODE 93792
|
Patient/caregiver training for initiation of home INR monitoring under the direction of a physician or other qualified health care professional, face-to-face, including use and care of the INR monitor, obtaining blood sample, instructions for reporting home INR test results, and documentation of patient's/caregiver's ability to perform testing and report results.
|
|
INR HOME MONITORING
|
CPT CODE 93793
|
Anticoagulant management for a patient taking warfarin, must include review and interpretation of a new home, office, or lab INR test result, patient instructions, dosage adjustment (as needed), and scheduling of additional test(s), when performed.
|
|
INR HOME MONITORING
|
HCPCS CODE G0248
|
Demonstration, prior to initiation of home INR monitoring, for patient with either mechanical heart valve(s), chronic atrial fibrillation, or venous thromboembolism who meets Medicare coverage criteria, under the direction of a physician; includes: face-to-face demonstration of use and care of the INR monitor, obtaining at least one blood sample, provision of instructions for reporting home INR test results, and documentation of patient's ability to perform testing and report results.
|
|
INR HOME MONITORING
|
HCPCS CODE G0249
|
Provision of test materials and equipment for home INR monitoring of patient with either mechanical heart valve(s), chronic atrial fibrillation, or venous thromboembolism who meets Medicare coverage criteria; includes: provision of materials for use in the home and reporting of test results to physician; testing not occurring more frequently than once a week; testing materials, billing units of service include four tests.
|
|
INR HOME MONITORING
|
HCPCS CODE G0250
|
Physician review, interpretation, and patient management of home INR testing for patient with either mechanical heart valve(s), chronic atrial fibrillation, or venous thromboembolism who meets Medicare coverage criteria; testing not occurring more frequently than once a week; billing units of service include four tests.
|
INR clinical quality measure:
The percentage of members 18 years of age and older who had at least one 56-day interval of warfarin therapy and who received at least one international normalized ratio (INR) monitoring test during each 56-day interval with active warfarin therapy.
|
Clinical Quality Measure
|
Required documentation
|
CPT, HCPCS, LOINC and CPT Performance Codes
|
Provider Specialty
|
|
INR Monitoring for Individuals on Warfarin*
|
Adults 18 years of age and older who have had at least one 56- day interval of warfarin therapy and received at least one INR monitoring test during each 56-day interval with active warfarin therapy in the measurement year. Excludes patients who are monitoring INR at home during the treatment period
|
CPT 85610 - Prothrombin time
LOINC 34714-6 INR blood by coagulation assay
6301-6 INR in platelet poor plasma by coagulation assay
38875-1 INR in platelet poor plasma or blood by coagulation assay
46418-0 INR in capillary blood by coagulation assay
52129-4 INR in platelet poor plasma by coagulation - post heparin adsorption
Excludes:
G0248 - demonstrate use home INR monitoring
G0249 - provide test materials and equipment for home INR monitoring
G0250 - physician INR test review interpretation and management
|
No provider type restrictions
|
In a recent study published by Pediatrics1, economic hardship, school closing and shutdowns led to sedentary lifestyles and increases in childhood obesity. The research analyzed doctor visits pre-pandemic then during the pandemic period and the increases were dramatic. Overall obesity increased from 13.7% to 15.4%. Increases observed ranged from 1% in children aged 13 to 17 years to 2.6% for those aged 5 to 9 years.
The study recommended new approaches to Weight Assessment and Counseling. These include recommending virtual activities that promote increased physical activity. Focusing on ways to remain safe and active with outside activities, such as park visits, walks and bike riding were also suggested.
The Centers for Disease Control and Prevention has a great resource, “Ways to promote health with preschoolers.” This fun flyer shows how we can all work together to support a healthy lifestyle. You can download a copy here.

The HEDIS® measure Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents (WCC) requires a nutritional evaluation and pro-active guidance as part of a routine health visit.
- When counseling for nutrition, document current nutritional behavior, such as meal patterns, eating and diet habits, and weight counseling.
- When counseling for physical activity, document current physical activity behavior, such as exercise routine, participation in sports activities, bike riding and play groups.
- Handouts about nutrition and physical activity also count toward meeting this HEDIS measure when documented in the member’s health record.
HEDIS® measure WCC looks at the percentage of members, 3-17 years of age, who had an outpatient visit with a PCP or OB/GYN and have documented evidence for all the following during the measurement year:
- Body mass index (BMI) percentile (percentage, not value)
- Counseling for nutrition
- Counseling for physical activity
Telehealth, virtual check-in, and telephone visits all meet the criteria for nutrition and physical activity counseling. Counseling does not need to take place only during a well-visit, WCC can also be completed during sick visits. Documenting guidance in your patient’s records is key.
Code services correctly to measure success
These diagnosis and procedure codes are used to document BMI percentile, weight assessment, and counseling for nutrition and physical activity:
|
Description
|
CPT®
|
ICD-10-CM
|
HCPCS
|
|
BMI percentile
|
|
Z68.51-Z68.54
|
|
|
Counseling for nutrition
|
97802, 97803,
97804
|
Z71.3
|
G0270, G0271, G0447, S9449,
S9452, S9470
|
|
Counseling for physical activity
|
|
Z02.5, Z71.82
|
G0447, S9451
|
|
Codes to identify outpatient visits:
CPT — 99201-99205, 99211-99215, 99241-99245, 99341-99345, 99347-99350, 99381-99387, 99391-99397, 99401-99404, 99411, 99412, 99429, 99455, 99456, 99483
HCPCS — G0402, G0438, G0439, G0463, T1015
|
|
ATTACHMENTS (available on web): 1232 image.jpg (jpg - 0.12mb) Many members have both primary and secondary insurance policies, and it’s important to know which policy is primary. We want to make it as easy as possible for you to find out so you can avoid claim denials for not filing the secondary claim within the timely filing guidelines.
Before the member arrives for their appointment, check the primary insurance carrier using the Eligibility and Benefits app in Availity. Log onto Availity.com, go to payer spaces, select us as the payer and use the Patient Registration tab to run an Eligibility and Benefits Inquiry. If you find that we are the primary payer, confirm that when the member arrives for their appointment. After providing services, submit the member’s claim as usual – you can use Availity for that, too, through the Claims & Payments app.
If we are the secondary payer, we will need the explanation of benefits (EOB) from the primary carrier along with the claim submission to determine our payment amount. You can submit the EOB and the claim through Availity using the Claims & Payments app.
When a claim is submitted to us as the primary payer, and we are the secondary payer, our claim system will deny the claim because we don’t have the EOB. This can cause a delay in receipt of your payment and can even cause you to miss the timely filing guideline.
We want you to have of the information you need to know the very best way to file your claims. For more information about filing claims, visit Anthem.com/provider/claims-submissions. For help using Availity, log onto Availity.com and select the Help & Training tab.
CMS average sales price (ASP) third quarter fee schedule with an effective date of July 1, 2021 will go into effect with Anthem Blue Cross and Blue Shield (Anthem) on August 1, 2021. To view the ASP fee schedule, please visit the CMS website at cms.hhs.gov/McrPartBDrugAvgSalesPrice/.
Effective for dates of service on and after October 1, 2021, Anthem Blue Cross and Blue Shield (Anthem) will increase the reimbursement penalty for failure to comply with the utilization management (UM) program’s prior authorization requirements for services rendered to commercial plan members. Late prior authorizations, and late notices in the case of emergency admissions, are currently subject to a penalty and will be subject to the increase in the penalty . Failure to comply with Anthem’s prior authorization requirements, and late notice requirements in the case of emergency admissions, will result in a 100% reduction in reimbursement to the provider and facility.
As a reminder, Anthem requires prior authorization prior to the delivery of certain elective services in both the inpatient and outpatient settings. For an emergency admission, prior authorization is not required; however, you must notify Anthem of the admission within the timeframe specified in the Provider Manual or as otherwise required by law. Failure to give timely notification for emergency admissions will also result in reimbursement penalties of 100% to providers and facilities.
Enforcement of the program requirement will lead to greater consistency in our processes. This notice updates Anthem’s UM program reimbursement penalties and the corresponding sections of the Provider Manual to reflect this change to the reimbursement penalty for non-compliance. As a reminder, providers and facilities may not balance bill the member for any such reduction in payment.

Join us throughout the year in a new Continuing Medical Education (CME) webinar series as we share practices and success stories to overcoming barriers in achieving clinical quality goals, attaining better patient outcomes and improving Star ratings.
Program objectives:
- Learn strategies to help you and your healthcare team improve your performance across a range of clinical areas including telehealth, pharmacy measures, chronic disease monitoring, cancer screenings, documentation and more.
- Apply the knowledge you gain from the webinars to improve your organization’s quality.
Attendees will receive one CME credit upon completion of a program evaluation at the conclusion of each webinar.
REGISTER HERE for our upcoming clinical quality webinars!
Anthem Blue Cross and Blue Shield (Anthem) uses Availity as its exclusive partner for managing all electronic data interchange (EDI) transactions.
When your organizations claims are submitted either by your clearinghouse/vendor or submitted directly using practice management software, it’s important to review and utilize all responses to understand where your claims are in the adjudication process and if any action is required.
Below is a summary of the process for electronic files, and the response reports that are returned by Availity:
Electronic file is submitted to Availity
- Availity acknowledges receipt of file and validates for X12 format in a series of responses.
- The series of initial responses indicate whether an electronic file was successfully received in correct format and accepted by Availity.
- If errors occur, the impacted file will require resubmission to Availity.
- If your organization uses a clearinghouse/vendor, they are responsible for reviewing these response files.
HIPAA and business validation
- Electronic Batch Report (EBR) – This response acknowledges accepted claims and identifies claims with a HIPAA and business edits prior to routing for adjudication.
- Impacted claims require resubmission to view on payer spaces Remittance Inquiry Tool and the (835) Electronic Remittance Advice. (Edit examples include - Invalid subscriber ID for the date of service and invalid billing and coding per industry standards)
- Clearinghouse/vendors may provide their own version of this report to your organization.
Availity routes claims to payer Anthem
- Delayed Payer Report (DPR) – This response file contains an additional level of editing by the membership adjudication system.
- Currently this response only returns for the Medicare/ Medicaid lines of business.
- The commercial lines will return this response in the future, look for forthcoming communications with the details.
- Impacted claims require resubmission to view on payer spaces Remittance Inquiry Tool and the (835) Electronic Remittance Advice.
- Clearinghouses/vendors may provide their own version of this report to your organization.
If you have further questions on the response reports, please contact Availity at 800-282-4548.
Like the payroll direct deposit service that most businesses offer their employees, electronic funds transfer (EFT) is a digital payment solution that uses the automated clearinghouse (ACH) network to transmit health care payments from a health plan to a health care provider’s bank account. Health plans can use a provider’s banking information only to deposit funds, not to withdraw funds.
Anthem Blue Cross and Blue Shield (Anthem) expects providers to accept payment via EFT in lieu of paper checks. Providers can register or manage account changes for EFT via the CAQH enrollment tool called EnrollHub™. This tool will help eliminate the need for paper registration, reduce administrative time and costs and allows physicians and facilities to register with multiple payers at one time. By eliminating paper checks, EFT payments are deposited directly into your account faster.
Read more about going digital with Anthem in the Provider Digital Engagement Supplement available online. Go to anthem.com, select Providers, under the Provider Resources heading select Forms and Guides. Pick your state if you haven’t done so already. From the Category drop down, select Digital Tools, then Provider Digital Engagement Supplement.
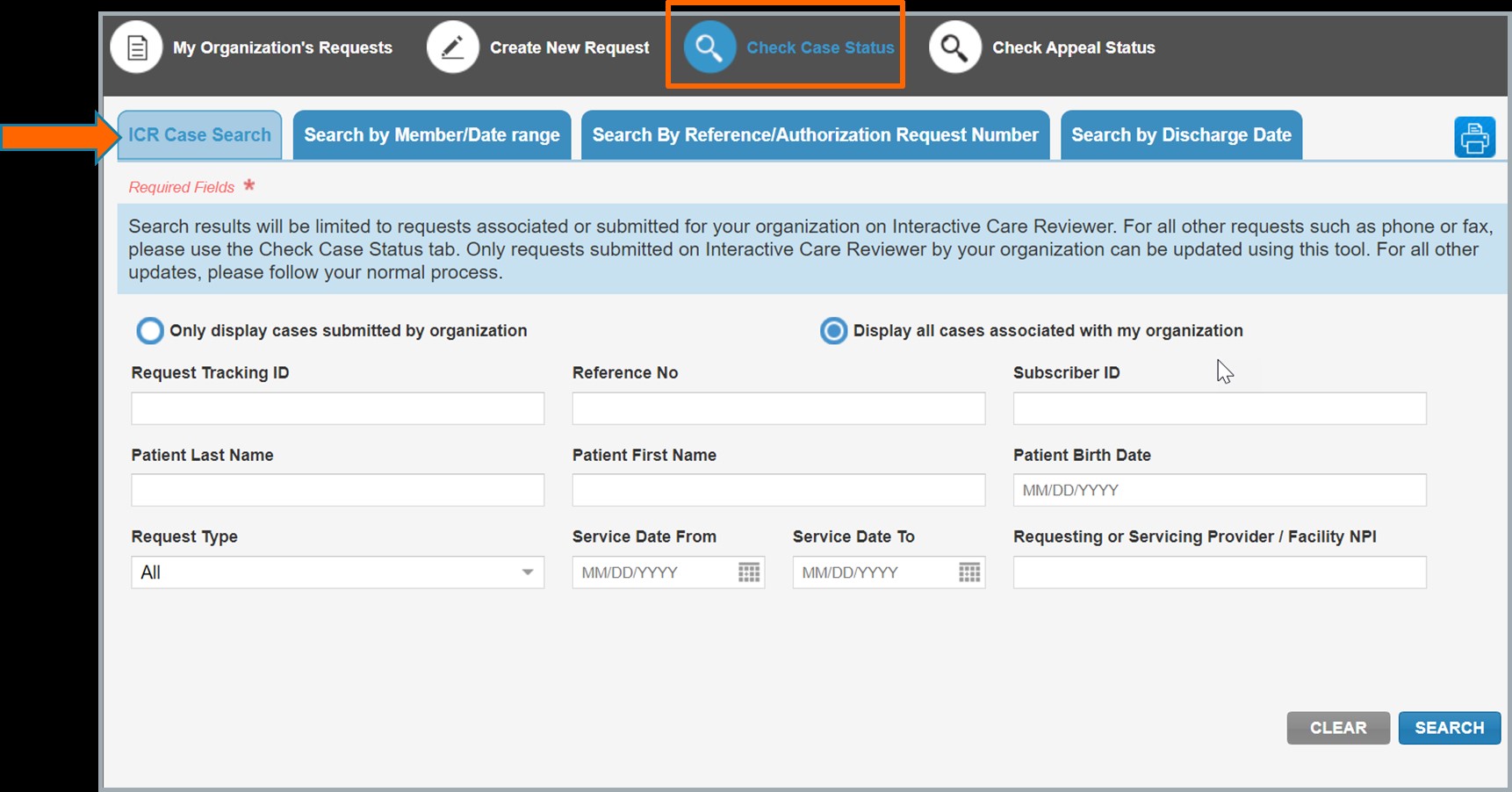
Locating a case using Interactive Care Reviewer (ICR), the Anthem Blue Cross and Blue Shield (Anthem) digital authorization tool just got easier. We added the ICR Case Search tab within the tool so you can find cases submitted through ICR. Cases submitted through both ICR and other sources can still be located using the other search options: member, date range, reference/authorization request number or discharge date.
The steps to access ICR through the Availity portal have not changed. You are required to have the Authorization & Referral Request role or the Authorization & Referral Inquiry role. Your organization’s
Availity administrator can assign these roles.
- Log onto Availity’s home page with your unique user ID and password
- Select Patient Registration
- Select Authorizations & Referrals
- Select Authorization Inquiry
- Choose the Payer and Organization
- Accept the ICR Disclaimer
- Select Check Case Status from the ICR navigation bar
Here is what’s new:
The ICR Inquiry dashboard displays the new ICR Case Search tab. This new option is currently available for users who have the Authorization & Referral Request role. Users with the Authorization & Referral Inquiry role will be able to access the ICR Case Search tab in mid-July. Until then, the additional search options are available.
To locate a case submitted through ICR, select the ICR Case Search tab then choose the criteria to complete your search.
You can use the additional search options to find cases requested by and associated with your organization that were submitted through both ICR and other sources.
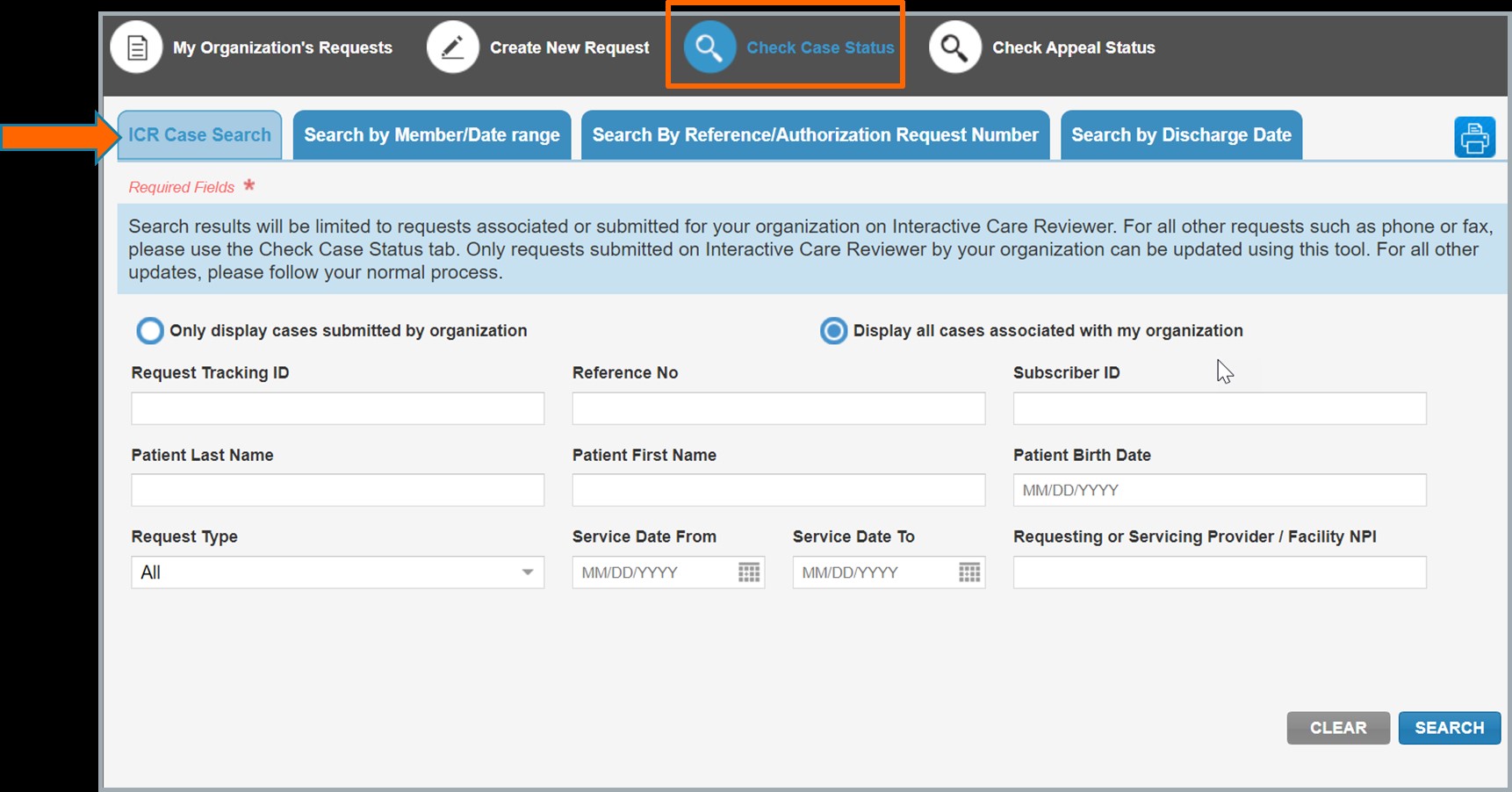
Use the additional search options to find cases through both ICR and other sources.
Register for our monthly new user ICR webinar to learn about basic navigation and features: ICR webinar registration
You can also visit the Custom Learning Center located on Availity Payer Spaces to access ICR navigation demonstrations and reference guides.
ATTACHMENTS (available on web): 1233 image.jpg (jpg - 0.21mb) Beginning with dates of service on or after October 1, 2021, Anthem Blue Cross and Blue Shield (Anthem) will implement a new reimbursement policy titled Non-Patient Laboratory Services. Anthem does not allow reimbursement for non-patient laboratory services when reported on a UB-04 with bill type 014X unless provider, state, federal or CMS and/or requirements indicate otherwise.
For more information about this policy, visit the Reimbursement page on our anthem.com/provider website.
Beginning with dates of service on or after October 1, 2021, Anthem Blue Cross and Blue Shield’s (Anthem’s) current documentation and reporting guidelines for consultations policy will be renamed “Consultations.” This policy aligns with CMS guidance and does not allow reimbursement for inpatient (99251-99255) or outpatient (99241-99245) consultation codes, and requires providers to bill the appropriate office visit Evaluation and Management (E/M) code for consultation services.
For more information about this policy, visit the Reimbursement page on our anthem.com/provider website.
For more than a decade, Blue Precision, Anthem Blue Cross and Blue Shield’s physician transparency program, has recognized specialists for meeting or exceeding established quality and cost effectiveness measures. Thank you to all those physicians participating in our networks and for the care you provide to our members.
Anthem is announcing that we have made the decision to retire our Blue Precision program effective December 31, 2021. Blue Precision recognition icons and other program information will be removed from anthem.com and our “Find Care” provider tool by January 1, 2022.
Going forward, Anthem will continue to focus and expand our consumer tools and content to assist members in making more informed and personalized healthcare decisions. We look forward to working collaboratively with you in other physician programs to provide our members with continued access to affordable and quality healthcare.
As previously communicated in the Anthem Blue Cross and Blue Shield (Anthem) May 2021 edition of Provider News, the AIM Rehabilitative program will be enhanced. Effective August 1, 2021, AIM Specialty Health ® (AIM), a separate company, will expand the AIM rehabilitative program to perform medical necessity review of the requested site of service for physical, occupational and speech therapy procedures for Anthem fully insured members.
AIM will require prior authorization for all outpatient facility and office-based rehabilitative and habiliative services. Prior authorization is recommended for the initial evaluation service codes, unless otherwise prohibited, to alert the provider of the site of care program and ensure the member is receiving care at the appropriate site of service early in the process. After the evaluation, ongoing services will be subject to site of care review and require prior authorization, including post service review which may result in a denial of coverage for not medically necessary for the site of care. Requests that are not medically necessary at a hospital site may be approved for coverage at a free standing or office-based setting. AIM will use the following Anthem clinical UM guidelines: CG-REHAB-10 Site of Care: Outpatient Physical Therapy, Occupational Therapy, and Speech-Language Pathology Services. The clinical criteria to be used for these reviews can be found on the anthem.com clinical UM guidelines page. Please note, this does not apply to procedures performed in an inpatient or observation setting, or on an emergent basis, members currently in an episode of care at the start of the program, or services with diagnosis of autism.
AIM will begin accepting prior authorization requests on July 19, 2021 for services provided on or after August 1, 2021. Prior authorization requests may be submitted via the AIM ProviderPortalSM or by calling 866-714-1103, Monday–Friday, 8:00 a.m.–6:00 p.m. ET. Monday through Friday.
AIM rehabilitation educational information
The AIM provider portal helps you learn more and access helpful information and tools such as order entry checklists and CPT code lists. Anthem also invites you to take advantage of a free informational webinar that will introduce you to the program and the robust capabilities of the AIM ProviderPortal. Go to the AIM Rehabilitation microsite to access helpful information and register for an upcoming webinar on July 8th or 27th at 3:00 p.m. ET. If you have previously registered for other services managed by AIM, there is no need to register again.
We value your participation in our network and look forward to working with you to help improve the health of our members.
As part of our ongoing quality improvement efforts, Anthem Blue Cross and Blue Shield (Anthem) is updating our precertification processes for certain specialty medications. Effective August 2021, we may request additional documentation for impacted medications to determine medical necessity.
Upon request, providers shall submit documentation from the member’s medical record for each policy question flagged for documentation. A denial may result if documentation does not support medical necessity.
Should you have any questions, please refer to our Clinical Criteria policy webpage for specific medication criteria details, including documentation requirements.
|
Impacted Policy
|
Impacted Medication(s)
|
|
ING-CC-0153: Adakveo (crizanlizumab)
|
Adakveo
|
|
ING-CC-0065: Agents for Hemophiilia A and von Willebrand Disease
|
Advate, Adynovate, Afstyla, Alphanate, Eloctate, Esperoct, Helixate FS, Hemlibra, Hemofil-M, Humate-P, Jivi, Koate-DVI, Kogenate FS, Kovaltry, Monoclate-P, Novoeight, Nuwiq, Obizur, Recombinate, Wilate, Xyntha
|
|
ING-CC-0148: Agents for Hemophilia B
|
Alphanine SD, Alprolix, Bebulin, Benefix, Idelvion, Ixinity, Mononine, Profilnine SD, Rebinyn, Rixubis
|
|
ING-CC-0025: Aldurazyme (laronidase)
|
Aldurazyme
|
|
ING-CC-0073: Alpha-1 Proteinase Inhibitor Therapy
|
Aralast, Glassia, Prolastin-C, Zemaira
|
|
ING-CC-0028: Benlysta (belimumab)
|
Benlysta
|
|
ING-CC-0012: Brineura (cerliponase alfa)
|
Brineura
|
|
ING-CC-0137: Cablivi (caplacizumab-yhdp)
|
Cablivi
|
|
ING-CC-0041: Complement Inhibitors
|
Soliris, Ultomiris
|
|
ING-CC-0081: Crysvita (burosumab-twza)
|
Crysvita
|
|
ING-CC-0035: Duopa (carbidopa and levodopa enteral suspension)
|
Duopa
|
|
ING-CC-0029: Dupixent (dupilumab)
|
Dupixent
|
|
ING-CC-0069: Egrifta (tesamorelin)
|
Egrifta
|
|
ING-CC-0024: Elaprase (idursufase)
|
Elaprase
|
|
ING-CC-0173: Enspryng (satralizumab-mwge)
|
Enspryng
|
|
ING-CC-0051: Enzyme Replacement Therapy for Gaucher Disease
|
Cerezyme, Elelyso, Vpriv
|
|
ING-CC-0044: Exondys 51 (eteplirsen)
|
Exondys 51
|
|
ING-CC-0021: Fabrazyme (agalsidase beta)
|
Fabrazyme
|
|
ING-CC-0068: Growth hormone
|
Genotropin, Humatrope, Norditropin, Nutropin AQ, Omnitrope, Saizen, Serostim, Zomacton, Zorbtive
|
|
ING-CC-0034: Hereditary Angioedema Agents
|
Berinert, Cinryze, Firazyr, Haegarda, Kalbitor, Ruconest, Takhzyro
|
|
ING-CC-0188: Imcivree (setmelanotide)
|
Imcivree
|
|
ING-CC-0070: Jetrea (ocriplasmin)
|
Jetrea
|
|
ING-CC-0037: Kanuma (sebelipase alfa)
|
Kanuma
|
|
ING-CC-0057: Krystexxa (pegloticase)
|
Krystexxa
|
|
ING-CC-0018: Lumizyme (alglucosidase alfa)
|
Lumizyme
|
|
ING-CC-0013: Mepsevii (vestronidase alfa)
|
Mepsevii
|
|
ING-CC-0043: Monoclonal Antibodies to Interleukin-5
|
Cinqair, Fasenra, Nucala
|
|
ING-CC-0023: Naglazyme (galsulfase)
|
Naglazyme
|
|
ING-CC-0111: Nplate (romiplostim)
|
Nplate
|
|
ING-CC-0082: Onpattro (patisiran)
|
Onpattro
|
|
ING-CC-0077: Palynziq (pegvaliase-pqpz)
|
Palynziq
|
|
ING-CC-0049: Radicava (edaravone)
|
Radicava
|
|
ING-CC-0156: Reblozyl (luspatercept)
|
Reblozyl
|
|
ING-CC-0159: Scenesse (afamelanotide)
|
Scenesse
|
|
ING-CC-0149: Select Clotting Agents for Bleeding Disorders
|
Feiba, Novoseven
|
|
ING-CC-0079: Strensiq (asfotase alfa)
|
Strensiq
|
|
ING-CC-0008: Subcutaneous Hormonal Implants
|
Testopel
|
|
ING-CC-0084: Tegsedi (inotersen)
|
Tegsedi
|
|
ING-CC-0162: Tepezza (teprotumumab-trbw)
|
Tepezza
|
|
ING-CC-0170: Uplizna (inebilizumab)
|
Uplizna
|
|
ING-CC-0172: Viltepso (viltolarsen)
|
Viltepso
|
|
ING-CC-0022: Vimizim (elosulfase alfa)
|
Vimizim
|
|
ING-CC-0152: Vyondys 53 (golodirsen)
|
Vyondys 53
|
|
ING-CC-0017: Xiaflex (clostridial collagenase histolyticum) injection
|
Xiaflex
|
|
ING-CC-0033: Xolair (omalizumab)
|
Xolair
|
This is an update to the article published in the April 2021 edition of Provider News regarding Site of Care medical necessity reviews for long-acting colony-stimulating factors.
The program will no longer begin on August 1, 2021.
Please see below for the complete updated notice.
This service will no longer be in effect on or after August 1, 2021 for medical necessity review of the site of care that was to be required for the following long-acting colony-stimulating factors for oncology indications for Anthem Blue Cross and Blue Shield (Anthem) commercial plan members.
- Neulasta® & Neulasta Onpro® (pegfilgrastim)
- Fulphila® (pegfilgrastim-jmdb)
- Udenyca® (pegfilgrastim-cbqv)
- Ziextenzo® (pegfilgrastim-bmez)
- Nyvepria™ (pegfilgrastim-apgf)
Submit a request for review
There will be no changes for ordering providers whom submit prior authorization requests for the hospital outpatient site of care for these medications for dates of service on or after August 1, 2021 to AIM in one of the following ways:
- Access AIM ProviderPortalSM directly at providerportal.com. Online access is available 24/7 to process orders in real-time, and is the fastest and most convenient way to request authorization.
- Access AIM via the Availity web portal at availity.com
- Call the AIM contact center toll-free number: 877-291-0366, Monday–Friday, 7:00 a.m.–5:00 p.m. PT.
Please note, this review does not apply to the following plans: BlueCard®, Federal Employee Program® (FEP®), Medicaid, Medicare Advantage, Medicare supplemental plans. Providers can view prior authorization requirements for Anthem members on the clinical criteria webpage.
Providers should continue to verify eligibility and benefits for all members prior to rendering services.
If you have questions, please call the provider service phone number on the member’s ID card.
Note: In some plans “level of care” or another term such as “setting” or “place of service” may be the term used in benefit plans, provider contracts or other materials instead of or in addition to “site of care” and in some plans, these terms may be used interchangeably. For simplicity, we will hereafter use “site of care.”
Prior authorization updates
Effective for dates of service on and after October 1, 2021, the following specialty pharmacy codes from current or new clinical criteria documents will be included in our prior authorization review process.
Please note, inclusion of National Drug Code (NDC) code on your claim will help expedite claim processing of drugs billed with a Not Otherwise Classified (NOC) code.
To access the Clinical Criteria information, click here.
Prior authorization clinical review of non-oncology use of specialty pharmacy drugs is managed by the medical specialty drug review team. Review of specialty pharmacy drugs for oncology use is managed by AIM Specialty Health® (AIM).
|
Clinical Criteria
|
HCPCS or CPT Code(s)
|
Drug
|
|
*ING-CC-0195
|
J3490, J9999, C9399, J3590
|
Abecma
|
* Non-oncology use is managed by the medical specialty drug review team.
** Oncology use is managed by AIM.
Step therapy updates
Effective for dates of service on and after October 1, 2021, the following specialty pharmacy codes from current or new clinical criteria documents will be included in our existing specialty pharmacy medical step therapy review process.
To access the Clinical Criteria information, please click here.
Prior authorization clinical review of non-oncology specialty pharmacy drugs will be managed by medical specialty drug review team. Review of specialty pharmacy drugs for oncology use is managed by AIM Specialty Health® (AIM).
|
Clinical Criteria
|
Status
|
Drug(s)
|
HCPCS Codes
|
|
ING-CC-0020
|
Non-preferred
|
Tysabri
|
J2323
|
Medicaid
Managing illness can be a daunting task for our members. It is not always easy to understand test results, how to obtain essential resources for treatment, or who to contact with questions and concerns.
Anthem Blue Cross and Blue Shield Healthcare Solutions is available to offer assistance in these difficult moments with our Complex Care Management program. Our care managers are part of an interdisciplinary team of clinicians and other resource professionals there to support members, families, PCPs, and caregivers. The complex care management process uses the experience and expertise of the Care Coordination team to educate and empower our members by increasing self-management skills. The complex care management process can help members understand their illnesses and learn about care choices to ensure they have access to quality, efficient healthcare.
Members or caregivers can refer themselves or family members by calling the Customer Service number located on their ID card. They will be transferred to a team member based on the immediate need. Physicians can refer their patients by contacting us telephonically or through electronic means. We can help with transitions across levels of care so that patients and caregivers are better prepared and informed about healthcare decisions and goals.
You can contact us by phone at 844-396-2330. Case Management business hours are Monday to Friday from 8 a.m. to 5p.m. Pacific time.
This communication applies to Medicaid under Anthem Blue Cross and Blue Shield Healthcare Solutions and Medicare Advantage under Anthem Blue Cross and Blue Shield (Anthem).
CMS issued an Interoperability and Patient Access Policy to reduce the burden of certain administrative processes. The CMS policy requires providers to implement application programming interfaces (APIs) to improve the electronic exchange of healthcare data between patient, provider and payer. The policy reiterates that in partnership with the Office of the National Coordinator for Health Information (ONC), CMS identified Health Level 7® (HL7) as the foundational standard to support data exchange via secure API. Implementation of this CMS mandate is expected by July 1, 2021.
The Clinical Data Acquisition Group for Anthem integrates admission, discharge and transfer (ADT) data from facility providers, health information exchanges and third-party aggregators. ADT data exchange helps Anthem:
- Better support members with care coordination and discharge planning — leading to healthier outcomes for our members, your patients.
- Proactively manage care transitions to avoid waste.
- Close care gaps and educate members about appropriate care settings.
Anthem would like to digitally exchange HL7 ADT messaging data for our members using secure data collection and transmission capabilities currently in use by facility systems. Facilities with network connections through vendors or health information exchanges can integrate ADT data with Anthem through these channels as well. Near real-time HL7 ADT messaging data — or at least within 24 hours of admission, discharge or transfer — enables Anthem to most effectively manage care transitions.
Email the Clinical Data and Analytics team at ADT_Intake@Anthem.com to get started today.
Medicaid
(Effective 10/01/21)
Anthem Blue Cross and Blue Shield Healthcare Solutions does not allow pass-through billing for lab services. Claims appended with Modifier 90 and an office place of service will be denied unless provider, state, federal or CMS contracts and/or requirements indicate otherwise.
Reimbursement will be made directly to the laboratory that performed the clinical diagnostic laboratory test based on 100% of the applicable fee schedule or contracted/negotiated rate.
Modifier 90 is defined as when laboratory procedures are performed by a party other than the treating or reporting physician or other qualified healthcare professional. The procedure may be identified by adding Modifier 90 to the usual procedure number.
For additional information, please review the Modifier 90: Reference (Outside) Laboratory and Pass-Through Billing reimbursement policy at mediproviders.anthem.com/nv.
This communication applies to Medicaid under Anthem Blue Cross and Blue Shield Healthcare Solutions and Medicare Advantage under Anthem Blue Cross and Blue Shield (Anthem).
CMS issued an Interoperability and Patient Access Policy to reduce the burden of certain administrative processes. The CMS policy requires providers to implement application programming interfaces (APIs) to improve the electronic exchange of healthcare data between patient, provider and payer. The policy reiterates that in partnership with the Office of the National Coordinator for Health Information (ONC), CMS identified Health Level 7® (HL7) as the foundational standard to support data exchange via secure API. Implementation of this CMS mandate is expected by July 1, 2021.
The Clinical Data Acquisition Group for Anthem integrates admission, discharge and transfer (ADT) data from facility providers, health information exchanges and third-party aggregators. ADT data exchange helps Anthem:
- Better support members with care coordination and discharge planning — leading to healthier outcomes for our members, your patients.
- Proactively manage care transitions to avoid waste.
- Close care gaps and educate members about appropriate care settings.
Anthem would like to digitally exchange HL7 ADT messaging data for our members using secure data collection and transmission capabilities currently in use by facility systems. Facilities with network connections through vendors or health information exchanges can integrate ADT data with Anthem through these channels as well. Near real-time HL7 ADT messaging data — or at least within 24 hours of admission, discharge or transfer — enables Anthem to most effectively manage care transitions.
Email the Clinical Data and Analytics team at ADT_Intake@Anthem.com to get started today.
Mental disorders among children may cause serious changes in the way children typically learn, behave or handle their emotions, which cause distress and problems getting through the day. Healthcare professionals use the guidelines in the American Psychiatric Association’s Diagnostic and Statistical Manual, Fifth Edition (DSM-5),1 to help diagnose mental health disorders in children.
The most common mental disorders of childhood and adolescence fall into the following categories:
- Anxiety disorders (generalized anxiety disorder, obsessive-compulsive disorder, panic disorder, phobic disorder)
- Depression
- Posttraumatic stress disorder (PTSD)
- Separation anxiety disorder
- Social anxiety disorder
- Obsessive-compulsive disorder
- Bipolar disorder
- Disruptive behavioral disorders (attention-deficit/hyperactivity disorder [ADHD], conduct disorder, and oppositional defiant disorder)
- Eating disorders
- Schizophrenia (less common).
Other conditions and concerns that affect children’s learning, behavior and emotions include learning and developmental disabilities, autism, and risk factors like substance use and self-harm.
ICD-10-CM coding:
- Chapter 5 of the ICD-10-CM code set categorizes mental disorders.
- Codes from chapter 5 are assigned based on the express documentation of the provider’s clinical judgment regarding the patient’s mental or behavioral disorder(s). The codes are not assigned based on symptoms, signs, or abnormal clinical laboratory findings.
Affective disorders
Major depressive disorder (MDD) is classified in ICD-10-CM as:
- F32: Major depressive disorder, single episode
- F33: Major depressive disorder, recurrent
When documenting major depressive disorder, keep in mind that proper and specific coding requires clear documentation of the:
- Episode: single versus recurrent.
- Severity: mild, moderate, or severe.
- Psychotic features, when present.
- Status of remission as either partial or full.
Remember to document any established causality between multiple mental health conditions. For example:
- Suppose the patient has a diagnosis of depression and a diagnosis of anxiety with a causal relationship between the two conditions. In such cases, documentation must establish the relationship by stating depression with, due to, or related to anxiety
ICD-10-CM classifies bipolar disorders under the following categories:
- F30: Manic episode (bipolar disorder, single manic episode, and mixed affective episode)
- F31: Bipolar disorder (manic-depressive illness, manic-depressive psychosis, and manic-depressive reaction)
- F34: Persistent mood affective disorders (cyclothymic disorder and dysthymic disorder)
- F39: Unspecified mood affective disorder (affective psychosis not otherwise specified).
Nonpsychotic mental disorders
Anxiety, dissociative, stress-related, somatoform and other nonpsychotic mental disorders are classified in categories F40 to F48.
Anxiety disorders are classified in ICD-10-CM under the following categories:
- F40: Phobic anxiety disorders
- F41: Other anxiety disorders
- F42: Obsessive-compulsive disorder.
Reactions to stress
ICD-10-CM provides category F43 for coding reactions to severe stress and adjustment disorders. Code F43.0, Acute stress reaction, classifies acute reaction to stress, including acute crisis reaction, crisis state, and psychic shock.
Posttraumatic stress disorder (PTSD) is classified in ICD-10-CM to subcategory F43.1, with
fifth-characters for unspecified, acute, or chronic.
Adjustment disorders are classified to subcategory F43.2, with the fifth-character axis being the nature of the reaction, such as anxiety, depression, or other symptoms. For example:
- 24: Child adopted from a foreign country, suffering from culture shock with conduct disturbance.
Behavioral syndromes associated with physiological disturbances and physical factors
Categories F50 to F59 are devoted to behavioral syndromes associated with physiological disturbances and physical factors. These codes are not assigned when the conditions are present due to mental disorders classified elsewhere or organic in origin. This grouping includes, for example:
- : Eating disorders (such as anorexia nervosa and bulimia nervosa)
- : Sleep disorders, not due to a substance or known physiological condition
- F54*: Psychological and behavioral factors associated with disorders or diseases classified elsewhere
F59: Unspecified behavioral syndromes associated with physiological disturbances and physical factors
* Code F54 classifies psychological and behavioral factors associated with diseases classified elsewhere. Typical conditions that are often associated with code F54 include asthma and dermatitis.
Schizophrenic disorders:
- Those types of disorders are classified in category F20, with a fourth character indicating the type of schizophrenia.
- The codes from category F20 are followed by an excludes one note indicating they should not be reported with codes classifying a brief psychotic disorder (F23) , cyclic schizophrenia (F25.0), schizoaffective disorder (F25-F25.9) and schizophrenic reaction not otherwise specified (NOS) (F23).
- Assign code F20.9, Schizophrenia, unspecified, for chronic schizophrenia with acute exacerbation. The existing ICD-10-CM codes for schizophrenia do not differentiate severity or an acute exacerbation (AHA Coding Clinic, Second Quarter 2019, p.32).
Attention deficit hyperactivity disorder (ADHD)
ICD-10-CM codes for ADHD include:
- 0: Attention-deficit hyperactivity disorder, predominantly inattentive type.
- 1: Attention-deficit hyperactivity disorder, predominantly hyperactive type.
- 2: Attention-deficit hyperactivity disorder, combined type.
- 8: Attention-deficit hyperactivity disorder, other types.
- 9: Attention-deficit hyperactivity disorder, unspecified type.
The ADHD diagnosis may not be established at the time of the initial physician office visit. Therefore, it may take two or more visits before the diagnosis is confirmed or ruled out.
ICD-10-CM outpatient coding guidelines specify not to assign a diagnosis code when documented as rule out, working diagnosis or other similar terms indicating uncertainty.
Instead, the outpatient coding guidelines instruct to code the condition(s) to the highest degree of certainty for that encounter/visit, requiring the use of codes that describe symptoms, signs or another reason for the visit.
History codes (categories Z80 to Z87) may be used as secondary codes if the historical condition or family history impacts current care or influences treatment. Personal and family history of ADHD has an impact on the clinical assessment of an individual for this disorder; the ICD-10-CM codes to report the history of ADHD in an individual include:
- 59: Personal history of other mental and behavioral disorders.
- 8: Family history of other mental and behavioral disorders.
Psychosocial circumstances
ICD-10-CM provides codes for behaviors that are not classified as behavioral disorders, such as:
- 840: Attention and concentration deficit
- 83: Excessive crying of child, adolescent, or adult
- 87: Impulsiveness
- 81: Obsessive-compulsive behavior.
MedicaidWell-child visits and vaccinations are essential services
In May 2020, the CDC released a report showing a drop in routine childhood vaccinations as a result of COVID-19; a result of stay-at-home orders and concerns about infection during well-child visits. Both the American Academy of Pediatrics and the CDC recommend the continuation of routine childhood vaccinations during the COVID-19 pandemic, noting they are essential services.
To encourage well-visits and vaccinations, here are some extra steps you can take to ensure visits are as safe as possible for both patients and staff. They include:
- Scheduling sick visits and well-child visits during different times of the day.
- Asking patients to remain outside until it’s time for their appointment to reduce the number of people in waiting rooms.
- Offering sick visits and well-child visits in different locations.
It is important to identify those children who have missed immunizations and well-child visits to schedule these essential in-person appointments. To help, the CDC has published vaccine catch-up guidance on their website.
Help your patients earn rewards
For additional encouragement, Anthem Blue Cross and Blue Shield Healthcare Solutions (Anthem) members can earn $25 or more in gift cards for completing vaccines and/or well visits through our Healthy Rewards program. Please encourage your patients to enroll in the program on the Anthem website so they can earn rewards for these activities.
See chart below:
|
Anthem
|
Childhood Immunization Status Combo 10 (CIS-10)
|
Child and Adolescent Well Care Visits (WCV)
|
|
Ages
|
0 to 1 (before 2nd birthday)
|
15 months to 19 years
|
|
Reward amount
|
$25
|
$25
|
Patients can enroll online at mss.anthem.com/nv or by calling 1-888-990-8681 (TTY).
Helpful information for keeping babies and children healthy:
Childhood Immunization Status (CIS) Combination 10 HEDIS® measure requires that all children are immunized by their 2nd birthday:
- Four DTap (diphtheria, tetanus and acellular pertussis)
- Three IPV (polio)
- One MMR (measles, mumps, rubella)
- Three HiB (H influenza type B)
- Three Hep B (hepatitis B)
- One VZV (chicken pox)
- Four PCV (pneumococcal conjugate)
- One Hep A (hepatitis A)
- Two or three RV (rotavirus)
- Two influenza (flu)
Billing codes:
- MMR:
- CPT®: 90707, 90710
- ICD-10-CM: B05.0-4, B05,81, B05.89, B05.9
- Mumps:
- ICD-10-CM:0-3, B26.81-85, B26.89, B26.9
- Rubella:
- ICD-10-CM:-00-02, B06.09, B06.81-82, B06.89, B06.9
- CPT: 90706
- Rubella antibody:
- Hepatitis A:
- CPT: 90633
- ICD-10-CM:0, B15.9
- Influenza:
- CPT: 90655, 90657, 90662, 90673, 90685, 90686-90689
- HCPCS: G0008
- Rotavirus vaccine (RV):
- CPT: 90681 (two-dose), 90680 (three-dose)
Children should be fully immunized by 13 years of age to meet the Immunization for Adolescents (IMA) Combination 2 HEDIS measure:
- One meningococcal vaccine (MCV) injection between 11 and 13 years of age
- One tetanus, diphtheria toxoids and acellular pertussis vaccine (Tdap/Td) between 10 and 13 years of age
- Two or three HPV vaccines between 9 and 13 years of age
Billing codes:
- Meningococcal:
- Tdap:
- HVP:
Please refer to the Anthem HEDIS coding booklet for coding guidelines.
MedicaidWhat Matters Most: Improving the Patient Experience is an online course for providers and office staff that addresses gaps in care and offers approaches to communication with patients. This course is available at no cost and is eligible for one CME credit by the American Academy of Family Physicians.
The What Matters Most training can be accessed at patientexptraining.com.
MedicaidAs patient panels grow more diverse and needs become more complex, providers and office staff need more support to help address patients’ needs. Anthem Blue Cross and Blue Shield Healthcare Solutions
(Anthem) wants to help.
Cultural competency resources
Here is an overview of the cultural competency resources available on our provider website.
- Cultural Competency and Patient Engagement includes:
- The impact of culture and cultural competency on healthcare.
- A cultural competency continuum, which can help providers assess their level of cultural competency.
- Disability competency and information on the Americans with Disabilities Act (ADA).
- Caring for Diverse Populations Toolkit includes:
- Comprehensive information, tools and resources to support enhanced care for diverse patients and mitigate barriers.
- Materials that can be printed and made available for patients in provider offices.
- Regulations and standards for cultural and linguistic services.
- My Diverse Patients offers:
- A comprehensive repository of resources to providers to help support the needs of diverse patients and address disparities.
- Courses with free continuing education credit through the American Academy of Family Physicians.
- Free accessibility from any device (for example, desktop computer, laptop, phone or tablet), no account or login required.
To access these resources, go to providers.anthem.com/nv > Manuals, Directories, Training & More > Tutorials, Reference Guides and Other Resources.
In addition, providers can access Stronger Together, which offers free resources to support the diverse health needs of all people where they live, learn, work and play. These resources were created by our parent company in collaboration with national organizations and are available for you to share with your patients and communities.

ATTACHMENTS (available on web): 0224 image.jpg (jpg - 0.02mb) MedicaidIn a recent notification, we shared that effective May 1, 2021, the following codes would be included in our prior authorization review process. Please be advised that these codes will not be included in our prior authorization process at this time.
|
Clinical Criteria
|
HCPCS or CPT® code(s)
|
Drug
|
|
ING-CC-0182
|
J1756
|
Venofer
|
|
ING-CC-0182
|
J2916
|
Ferrlecit
|
|
ING-CC-0182
|
J1750
|
Infed
|
|
ING-CC-0182
|
J1439
|
Injectafer
|
|
ING-CC-0182
|
Q0138
|
Feraheme
|
|
ING-CC-0182
|
J1437
|
Monoferric
|
Medicare Advantage
On March 25, 2021, and April 8, 2021, the Pharmacy and Therapeutics (P&T) Committee approved the following clinical criteria applicable to the medical drug benefit for Anthem Blue Cross and Blue Shield. These policies were developed, revised, or reviewed to support clinical coding edits.
Visit clinical criteria to search for specific policies. If you have questions or would like additional information, use this email.
Please see the explanation/definition for each category of clinical criteria below:
- New: newly published criteria
- Revised: addition or removal of medical necessity requirements, new document number
- Updates marked with an asterisk (*) notate that the criteria may be perceived as more restrictive
Please share this notice with other members of your practice and office staff.
Note: The clinical criteria listed below applies only to the medical drug benefits contained within the member’s medical policy. This does not apply to pharmacy services.
|
Effective date
|
Document number
|
clinical criteria title
|
New or revised
|
|
July 16, 2021
|
ING-CC-0195*
|
Abecma (idecabtagene vicleucel)
|
New
|
|
July 16, 2021
|
ING-CC-0191*
|
Pepaxto (melphalan flufenamide; melflufen)
|
New
|
|
July 16, 2021
|
ING-CC-0192*
|
Cosela (trilaciclib)
|
New
|
|
July 16, 2021
|
ING-CC-0193*
|
Evkeeza (evinacumab)
|
New
|
|
July 16, 2021
|
ING-CC-0194*
|
Cabenuva (cabotegravir extended-release; rilpivirine extended-release) Injection
|
New
|
|
July 16, 2021
|
ING-CC-0125
|
Opdivo (nivolumab)
|
Revised
|
|
July 16, 2021
|
ING-CC-0064
|
Interleukin-1 Inhibitors
|
Revised
|
|
July 16, 2021
|
ING-CC-0159*
|
Scenesse (afamelanotide)
|
Revised
|
|
July 16, 2021
|
ING-CC-0151
|
Yescarta (axicabtagene ciloleucel)
|
Revised
|
|
July 16, 2021
|
ING-CC-0145*
|
Libtayo (cemiplimab-rwlc)
|
Revised
|
|
July 16, 2021
|
ING-CC-0130*
|
Imfinzi (durvalumab)
|
Revised
|
|
July 16, 2021
|
ING-CC-0127
|
Darzalex (daratumumab) and Darzalex Faspro (daratumumab and hyaluronidase-fihj)
|
Revised
|
|
July 16, 2021
|
ING-CC-0075*
|
Rituximab Agents for Non-Oncologic Indications
|
Revised
|
Medicaid
Our utilization management (UM) decisions are based on the appropriateness of care and service needed, as well as the member’s coverage according to their health plan. We do not reward providers or other individuals for issuing denials of coverage, service, or care. Nor do we make decisions about hiring, promoting, or terminating these individuals based on the idea or thought that they will deny benefits. In addition, we do not offer financial incentives for UM decision makers to encourage decisions resulting in underutilization. Our medical policies are available on our provider website at mediproviders.anthem.com/nv/pages/medical-policies.aspx.
You can request a free copy of our UM criteria from Provider Services at 844-396-2330. Providers can discuss a UM denial decision with a physician reviewer by calling us toll-free at the number listed below. To access UM criteria online, go to mediproviders.anthem.com/nv/pages/medical-policies.aspx.
We are staffed with clinical professionals who coordinate our members’ care and are available 24/7 to accept precertification requests. Secured voicemail is available during off-business hours. A clinical professional will return your call within the next business day. Our staff will identify themselves by name, title, and organization name when initiating or returning calls regarding UM issues.
You can submit precertification requests by:
- Fax:
- DME, physical therapy/occupational therapy/speech therapy, pain management, home care, home infusion requiring nursing services, insulin pumps, hyperbaric treatment, or wound care: 866-920-8362
- Inpatient services: 844-442-8009
- Outpatient services: 844-430-6807
- Pharmacy prior authorization, including home infusion injectables, continuous glucose monitoring equipment, and diabetic supplies: 844-490-4876
- Phone: 844-396-2330
- Pharmacy: 844-396-2330
- Availity* Portal: availity.com
Have questions about utilization decisions or the UM process?
Call our Clinical team at 844-396-2330 Monday through Friday from 8 a.m. to 5 p.m. Pacific time.
Medicaid
The Medical Policies, Clinical Utilization Management (UM) Guidelines and Third Party Criteria below were developed and/or revised to support clinical coding edits. Note, several policies and guidelines were revised to provide clarification only and are not included. Existing precertification requirements have not changed.
Please share this notice with other members of your practice and office staff.
To view a guideline, visit anthem.com/search.html.
Notes/updates:
Updates marked with an asterisk (*) notate that the criteria may be perceived as more restrictive.
- *CG-LAB-17 - molecular gastrointestinal pathogen panel (GIPP) testing for infectious diarrhea in the outpatient setting
- Outlines the medical necessity and not medically necessary criteria for multiplex PCR-based panel testing of gastrointestinal pathogens for infectious diarrhea in the outpatient setting
- *GENE.00056 - gene expression profiling for bladder cancer
- Gene expression profiling for diagnosing, managing and monitoring bladder cancer is considered investigational and not medically necessary
- *LAB.00038 - cell-free DNA testing to aid in the monitoring of kidney Transplants for rejection
- Cell-free DNA testing is considered investigational and not medically necessary as a non-invasive method of determining the risk of rejection in kidney transplant recipients
- *LAB.00039 - pooled antibiotic sensitivity testing
- Pooled antibiotic sensitivity testing is considered investigational and not medically necessary in the outpatient setting for all indications
- *SURG.00159 - focal laser ablation for the treatment of prostate cancer
- Focal laser ablation is considered investigational and not medically necessary for the treatment of prostate cancer
- *TRANS.00037 - uterine transplantation
- Uterine transplantation is considered investigational and not medically necessary for all uses, including but not limited to the treatment of uterine factor infertility due to nonfunctioning or absent uterus
- *ANC.00008 - cosmetic and reconstructive services of the head and neck
- Added otoplasty using a custom-fabricated device, including but not limited to a custom fabricated alloplastic implant, as cosmetic and not medically necessary
- *CG-OR-PR-04 - cranial remodeling bands and helmets (cranial orthotics)
- Removed condition requirement from reconstructive criteria and replaced current diagnostic reconstructive criteria with criteria based on one of the following cephalometric measurements: the cephalic index, the cephalic vault asymmetry index, the oblique diameter difference index, or the cranioproportional index of plagiocephelometry
- *CG-SURG-78 - locoregional and surgical techniques for treating primary and metastatic liver malignancies
- Added TACE using immunoembolization (for example, using granulocyte-macrophage colony-stimulating factor [GM-CSF]) as not medically necessary for all liver-related indications
- *CG-SURG-82 - bone-anchored and bone conduction hearing aids
- Revised audiologic pure tone average bone conduction threshold criteria for unilateral implant for bilateral hearing loss
- Added not medically necessary statement for when medical necessity criteria have not been met and clarified not medically necessary statement regarding replacement parts or upgrades
- Added bone conduction hearing aids using an adhesive adapter behind the ear as not medically necessary for all indications
- CG-GENE-22 - gene expression profiling for managing breast cancer treatment
- A new clinical guideline was created from the content contained in GENE.00011. There are no changes to the guideline content and the publish date is April 7, 2021.
- CG-GENE-23 - genetic testing for heritable cardiac conditions
- A new clinical guideline was created from the content contained in GENE.00007 and GENE.00017. There are no changes to the guideline content and the publish date is April 7, 2021
- CG-SURG-110 - lung volume reduction surgery
- A new clinical guideline was created from the content contained in SURG.00022. There are no changes to the guideline content and the publish date is June 25, 2021
AIM Specialty Health®* clinical appropriateness guideline updates.
To view AIM guidelines, visit the AIM Specialty Health page.
- The Small Joint Surgery Guideline has been revised and will be effective on March 14, 2021.
- The following Guidelines have been revised and will be effective on July 1, 2021:
- * Joint Surgery
- * Spine Surgery
Medical policies
On February 11, 2021, the Medical Policy and Technology Assessment Committee (MPTAC) approved the following medical policies applicable to Anthem Blue Cross and Blue Shield Healthcare Solutions
(Anthem). These guidelines take effect on July 1, 2021.
|
Publish date
|
Medical policy number
|
Medical policy title
|
New or revised
|
|
4/1/2021
|
*GENE.00056
|
Gene Expression Profiling for Bladder Cancer
|
New
|
|
4/7/2021
|
*LAB.00038
|
Cell-free DNA Testing to Aid in the Monitoring of Kidney Transplants for Rejection
|
New
|
|
4/7/2021
|
*LAB.00039
|
Pooled Antibiotic Sensitivity Testing
|
New
|
|
4/7/2021
|
*SURG.00159
|
Focal Laser Ablation for the Treatment of Prostate Cancer
|
New
|
|
4/7/2021
|
*TRANS.00037
|
Uterine Transplantation
|
New
|
|
4/7/2021
|
*ANC.00008
|
Cosmetic and Reconstructive Services of the Head and Neck
|
Revised
|
|
4/7/2021
|
MED.00087
|
Optical Detection for Screening and Identification of Cervical Cancer
|
Revised
|
|
2/18/2021
|
SURG.00121
|
Transcatheter Heart Valve Procedures
|
Revised
|
|
2/18/2021
|
SURG.00145
|
Mechanical Circulatory Assist Devices (Ventricular Assist Devices, Percutaneous Ventricular Assist Devices and Artificial Hearts)
|
Revised
|
Clinical UM guidelines
On February 11, 2021, the MPTAC approved the following clinical UM guidelines applicable to Anthem. These guidelines were adopted by the medical operations committee for Anthem members on February 25, 2021. These guidelines take effect on July 1, 2021.
|
Publish date
|
Clinical UM guideline number
|
Clinical UM guideline title
|
New or revised
|
|
4/7/2021
|
*CG-LAB-17
|
Molecular Gastrointestinal Pathogen Panel (GIPP) Testing for Infectious Diarrhea in the Outpatient Setting
|
New
|
|
2/18/2021
|
CG-GENE-21
|
Cell-Free Fetal DNA-Based Prenatal Testing
|
Revised
|
|
4/7/2021
|
CG-MED-26
|
Neonatal Levels of Care
|
Revised
|
|
2/18/2021
|
CG-MED-87
|
Single Photon Emission Computed Tomography Scans for Noncardiovascular Indications
|
Revised
|
|
4/7/2021
|
*CG-OR-PR-04
|
Cranial Remodeling Bands and Helmets (Cranial Orthotics)
|
Revised
|
|
2/18/2021
|
CG-SURG-55
|
Intracardiac Electrophysiological Studies (EPS) and Catheter Ablation
|
Revised
|
|
4/7/2021
|
CG-SURG-71
|
Reduction Mammaplasty
|
Revised
|
|
4/7/2021
|
*CG-SURG-78
|
Locoregional and Surgical Techniques for Treating Primary and Metastatic Liver Malignancies
|
Revised
|
|
4/7/2021
|
*CG-SURG-82
|
Bone-Anchored and Bone Conduction Hearing Aids
|
Revised
|
|
4/7/2021
|
CG-SURG-97
|
Cardioverter Defibrillators
|
Revised
|
Medicaid
The delivery of quality healthcare requires cooperation between patients, their providers, and their healthcare benefit plans. One of the first steps is for patients and providers to understand their rights and responsibilities. Therefore, in line with our commitment participating practitioners and members in our system, Anthem Blue Cross and Blue Shield Healthcare Solutions has adopted a Members’ Rights and Responsibilities Statement, which is located in the provider manual.
If you need a physical copy of the statement, call Provider Services at 844-396-2330.
Medicaid
Doluce David Ezeanolue, MD
David Ezeanolue, MD (Dr. Ez) is an experienced, multiple board-certified specialist who has practiced in Las Vegas since 1997. He graduated at the top of his medical school class and is widely respected as an excellent physician by his patients. He is an internationally recognized interventional pain specialist as well as a top 2 percentile board-certified internist (American Board of Internal Medicine). He has received numerous America’s Top Physician Awards from Consumer Research Council of America.
He is a Fellow of Interventional Pain Management (World Institute of Pain). He is also certified by the American Boards of Interventional Pain Practice, Internal Medicine, Electrodiagnostic Medicine, Addiction Medicine, Physical Medicine and Rehabilitation. Dr. Ez is also certified by the American Board of Certified Independent Medical Examiners.
Dr. Ez brings a wealth of experience to Apex Medical Center as he has amassed many impressive skills that he uses to treat patients from in and around Las Vegas and Henderson, Nevada. At Apex Medical Center, Dr. Ez is honored to put these skills and experience to use helping patients achieve their personal best in health and wellness. Working to find effective solutions for a wide range of physical ailments is also a driving force in his medical practice. His expertise, along with his personable nature, has earned Dr. Ez many loyal patients who turn to him in times of need.
Each quarter, we will feature one of our amazing providers. This feature is meant to highlight the diversity in our network and the membership we serve. We can also highlight shared best practices. If you would like to be considered, please email your Provider Experience consultant. You only need to write in once. We will revisit submissions each quarter. Thank you for all the work you do.
ATTACHMENTS (available on web): 0235 image.jpg (jpg - 0.03mb) Medicaid
Effective September 1, 2021, prior authorization (PA) requirements will change for 0205U, 0209U, and 0218U. The medical codes listed below will require PA from Anthem Blue Cross and Blue Shield Healthcare Solutions for Nevada Medicaid members. Federal and state law, as well as state contract language and CMS guidelines, including definitions and specific contract provisions/exclusions, take precedence over these PA rules and must be considered first when determining coverage.
Noncompliance with new requirements may result in denied claims.
PA requirements will be added to the following:
- 0205U — ophthalmology (age-related macular degeneration), analysis of 3 gene variants (2 CFH gene, 1 ARMS2 gene), using PCR and MALDI-TOF, buccal swab, reported as positive or negative for neovascular age-related macular-degeneration risk associated with zinc supplements
- 0209U — cytogenomic constitutional (genome-wide) analysis, interrogation of genomic regions for copy number, structural changes and areas of homozygosity for chromosomal abnormalities
- 0218U — neurology (muscular dystrophy), DMD gene sequence analysis, including small sequence changes, deletions, duplications, and variants in non-uniquely mappable regions, blood or saliva, identification and characterization of genetic variants
To request PA, you may use one of the following methods:
Not all PA requirements are listed here. Detailed PA requirements are available to contracted providers by accessing the provider self-service tool through the Availity* Portal at availity.com or by going to the provider website at providers.anthem.com/nv > Login. Contracted and noncontracted providers unable to access Availity can call Provider Services at 844-396-2330 for assistance with PA requirements.
Medicaid
Healthcare providers are seen as trusted sources of medical information and are in a unique position to improve lives and community health. Research shows that a strong vaccination recommendation from a provider is the greatest motivator for people of all ages to vaccinate themselves and their family members against serious infectious diseases.
Let’s Vaccinate offers providers tools and strategies to aid in vaccinating people of all ages. This website will help your practice:
- Address disparities for vaccine-preventable diseases.
- Identify and fill workflow gaps, including assessing vaccination status, enhancing vaccine, communications, providing vaccine education, and improving vaccine management and administration in your office.
- Access up-to-date guidance from the Centers for Disease Control and Prevention (CDC) for vaccines.
- Connect with your state immunization program, local immunization coalition, or other vaccine advocates in your community to collaborate.
Keeping all patients healthy and safe requires the support and collaboration of the entire healthcare industry. So, together, let’s vaccinate.
Medicaid
Effective September 1, 2021, prior authorization (PA) requirements will change for multiple codes. The medical codes listed below will require PA by Anthem Blue Cross and Blue Shield Healthcare Solutions for Nevada Medicaid members. Federal and state law, as well as state contract language and CMS guidelines, including definitions and specific contract provisions/exclusions, take precedence over these PA rules and must be considered first when determining coverage.
Noncompliance with new requirements may result in denied claims.
PA requirements will be added to the following:
- 0153U — oncology (breast), mRNA, gene expression profiling by next-generation sequencing of 101 genes, utilizing formalin-fixed paraffin-embedded tissue, algorithm reported as a triple negative breast cancer clinical subtype(s) with information on immune cell involvement
- 0244U — oncology (solid organ), DNA, comprehensive genomic profiling, 257 genes, interrogation for single-nucleotide variants, insertions/deletions, copy number alterations, gene rearrangements, tumor-mutational burden and microsatellite instability, utilizing formalin-fixed paraffin-embedded tumor tissue
- 81518 — oncology (breast), mRNA, gene expression profiling by real-time RT-PCR of 11 genes
(7 content and 4 housekeeping), utilizing formalin-fixed paraffin-embedded tissue, algorithms reported as percentage risk for metastatic recurrence and likelihood of benefit from extended endocrine therapy
- 81519 — oncology (breast), mRNA, gene expression profiling by real-time RT-PCR of 21 genes, utilizing formalin-fixed paraffin embedded tissue, algorithm reported as recurrence score
- 81522 — oncology (breast), mRNA, gene expression profiling by RT-PCR of 12 genes
(8 content and 4 housekeeping), utilizing formalin-fixed paraffin-embedded tissue, algorithm reported as recurrence risk score
To request PA, you may use one of the following methods:
Not all PA requirements are listed here. Detailed PA requirements are available to contracted providers by accessing the provider self-service tool on the Availity* Portal at availity.com or on the provider website at providers.anthem.com/nv > Login. Contracted and noncontracted providers who are unable to access Availity can call our Provider Services at 844-396-2330 for assistance with PA requirements.
Medicaid
We are committed to finding the best ways possible to support our members and providers, and we need your help. Please take a moment to complete the Behavioral Health Areas of Expertise Profile (BHAEP) online survey. This survey is designed to capture supplemental data to enhance our online provider directory and help members find the right behavioral health (BH) provider for their unique needs.
Do I have to complete this survey?
All BH practitioners contracted with Anthem Blue Cross and Blue Shield Healthcare Solutions will be asked to complete a survey. However, completion of this survey does not impact your credentialing materials, status, or provider contract. Any representation of a clinical area of interest is based on your self‑disclosure and professional judgment. Please only select those items that fall within the scope of your state‑issued license, clinical experience, and any certifications.
Where can I complete the online survey?
You can access the BHAEP online survey at https://tinyurl.com/BHAEP-Survey. You must complete a separate form for each clinical location. Please complete this survey as soon as possible. Your response is critical in helping us match the services you offer with our members’ needs.
What if I need assistance?
If you have any questions about completing the survey, please contact Provider Services at 844-396-2330. Any changes or amendments to your provider contract or credentialing must be requested through your Provider Experience representative.
We appreciate your continued support.
Medicaid
Please continue to check Medicaid Provider Communications & updates at anthem.com/nymedicaiddoc for the latest Medicaid information, including:
Medicare Advantage
(Effective 10/01/21)
Anthem Blue Cross and Blue Shield does not allow pass-through billing for lab services. Claims appended with Modifier 90 and an office place of service will be denied unless provider, state, federal or CMS contracts and/or requirements indicate otherwise.
Reimbursement will be made directly to the laboratory that performed the clinical diagnostic laboratory test based on 100% of the applicable fee schedule or contracted/negotiated rate.
Modifier 90 is defined as when laboratory procedures are performed by a party other than the treating or reporting physician or other qualified healthcare professional. The procedure may be identified by adding Modifier 90 to the usual procedure number.
For additional information, please review the Modifier 90: Reference (Outside) Laboratory and Pass-Through Billing reimbursement policy at anthem.com/medicareprovider.
ABSCRNU-0212-21
Medicare Advantage
Help increase your vaccination rates and close gaps-in-care with these tools and strategies
Healthcare providers are seen as trusted sources of medical information and are in a unique position to improve lives and community health. Research shows that a strong vaccination recommendation from a provider is the greatest motivator for people of all ages to vaccinate themselves and their family members against serious infectious diseases.
Let’s Vaccinate offers providers tools and strategies to aid in vaccinating people of all ages. This website will help your practice:
- Address disparities for vaccine-preventable diseases.
- Identify and fill workflow gaps, including assessing vaccination status, enhancing vaccine, communications, providing vaccine education, and improving vaccine management and administration in your office.
- Access up-to-date guidance from the Centers for Disease Control and Prevention (CDC) for vaccines.
- Connect with your state immunization program, local immunization coalition, or other vaccine advocates in your community to collaborate.
Keeping all patients healthy and safe requires the support and collaboration of the entire healthcare industry. So, together, let’s vaccinate.
Medicare Advantage
On October 1, 2021, prior authorization (PA) requirements will change for A0426 and A0428 covered by Anthem Blue Cross and Blue Shield. Federal and state law, as well as state contract language and CMS guidelines, including definitions and specific contract provisions/exclusions, take precedence over these precertification rules and must be considered first when determining coverage.
Noncompliance with new requirements may result in denied claims.
PA requirements will be added for the following codes:
- A0426 — ambulance service, advanced life support, nonemergency transport, level 1 (ALS 1)
- A0428 — ambulance service, basic life support, nonemergency transport (BLS)
Not all PA requirements are listed here. Detailed PA requirements are available to contracted providers by accessing the provider self-service tool on the Availity* Portal at availity.com or on the provider website at anthem.com/medicareprovider > Login. Contracted and noncontracted providers unable to access Availity can call the Provider Services located on the back of their patient’s member ID card for PA requirements.
|