Provider News MaineMay 1, 2019 May 2019 Anthem Maine Provider NewsletterAdministrativeAdministrative | Anthem Blue Cross and Blue Shield | Commercial | May 1, 2019 Good HbA1c <8State & FederalState & Federal | Anthem Blue Cross and Blue Shield | Medicare Advantage | May 1, 2019 Fall prevention tips
Diabetes is a complex chronic illness that requires monitoring on an ongoing basis. Currently, more than 23 million Americans are diagnosed with diabetes.1 The Centers for Disease Control shows diabetes as the 7th leading cause of death in the United States. In Maine approximately 142,000 people, or 11.5% of the adult population, have diabetes and 386,000 people, 37.2% of the adult population, have prediabetes with blood glucose levels higher than normal, but not yet high enough to be diagnosed as diabetes.2
Diabetes is expensive. In 2017, it accounted for $237 billion in direct medical costs.3 Diagnosed diabetes costs an estimated $1.4 billion in Maine each year. People with diabetes have medical expenses approximately 2.3 times higher than those who do not have diabetes and a myriad of co-existing conditions that contribute to these costs.4 The serious complications include heart disease, stroke, amputation, end-stage kidney disease, blindness – and death.5
Since diabetes HbA1c testing is a key measure to assess for future medical conditions related to complications of undiagnosed diabetes, the National Commission for Quality Assurance (NCQA) requires health plans to review claims for diabetes in patient health records and the findings contribute to health plan Accreditation levels and the Quality Rating System (QRS) measurement for Marketplace plans. A systematic sample of patient records is pulled annually as part of the HEDIS® medical record review to assess for documentation.
What is the HEDIS measure?
The diabetes measures focus on members 18-75 years of age with diabetes (type 1 and type 2) who had each of the following assessments:
- Hemoglobin A1c (HbA1c) testing
- HbA1c poor control (>9.0%)
- HbA1c control (<8.0%)
- Dilated retinal exam
- Medical attention for nephropathy
Each year NCQA reviews the measures and makes changes in accordance with technological or medical improvements. This year, NCQA also has updated the approach to allow for more administrative methods to collect the measure and added telehealth encounters to satisfy certain components of the measure. One of two patient visits may be a telehealth visit, a telephone visit or an online assessment. When documenting patients’ records, use the telehealth code from CPT II codes in combination with the diabetes diagnoses.
Continued management and diverse pathways to care are essential in controlling blood glucose and reducing the risk of complications. While it is extremely beneficial for the patient to have continuous management, it also benefits our providers. As HEDIS rates increase, there is potential for the provider to earn maximum or additional revenue through Pay for Quality, Value Based Services, and other pay-for-performance models.6
As part of our commitment to provide you with the latest clinical information and educational materials, we have adopted nationally recognized medical, behavioral health and preventive health guidelines which are available to providers on our website. The guidelines, which are used for our Quality programs, are based on reasonable, medical evidence, and are reviewed for content accuracy, current primary sources, the newest technological advances and recent medical research.
All guidelines are reviewed annually, and updated as needed. The current guidelines are available on our website at anthem.com/provider > scroll down and select ‘Find Resources for [state]’ > Health and Wellness > Practice Guidelines. As a contracted provider with Anthem, please remember that you are obligated when medically appropriate to refer our members to in-network providers. This includes physicians and all provider types including, but not limited to, ambulance transport (ground and air), ambulatory surgical centers, behavioral health services, physical medicine providers and ancillary providers. Referring to in-network providers allows members to receive the highest level of benefits under their Health Benefit Plan. As a reminder, call Anthem first for prior authorization if required by the member’s policy.
Ground Ambulance Providers
You can search for participating ground providers using our online tool, Provider Finder, located at anthem.com/provider. Search parameters include distance from your location (zip code, address or county). To use the tool, go to anthem.com/provider, scroll down and select ‘Find Resources for Maine’, and follow these steps in our “Find a Doctor” tool:
- Select “all plans/networks”
- Select type of coverage
- I am looking for a : “other medical services”
- Who specializes in: “ambulance companies”
- Located near: add your address, zip code or county
Air Ambulance Providers
The providers listed below are participating air ambulance providers with Anthem in Maine. This means that these providers have contractually agreed to accept the Anthem Rate as payment in full for covered services, and they will bill members only for allowable benefit cost-share obligations when transporting members who are picked up in Maine.
Some air ambulance providers choose not to participate with us.
- These air ambulance providers may charge members rates that are much higher than our contracted provider rates.
- Depending on their benefits, members who utilize non-participating air ambulance providers can be left with significant out-of-pocket expenses, which the ambulance providers and their billing agents may seek to collect.
To avoid these situations, we ask that, whenever possible, you use a participating air ambulance provider for your patients who are our members. Utilizing participating providers:
- Protects the member from balance billing for what may be excessive amounts,
- Assures the most economical use of the member’s benefits, and
- Is consistent with your contractual obligations to refer to in-network providers where available.
To schedule fixed wing or rotary wing air ambulance services, please contact us for prior authorization if required by the member’s policy, then call one of the phone numbers listed below. Please have the following information ready when you call:
- Basic medical information about the patient, including the patient’s name and date of birth or age. If the service was not prior authorized with Anthem, the air ambulance provider will also need to receive a full medical report from the attending facility.
- Current location of the patient, the name of the hospital or facility caring for the patient and its address (city and state)
- Location where patient is to be transported, including the name of the destination hospital/facility and address
- Approximate transport date or time frame
- Special equipment or care needs
Should you have questions regarding the air ambulance network, including providers contracted for air ambulance pickups outside of Maine, please contact the Provider Call Center.
Fixed Wing (Airplane) Providers (HCPCS Codes: A0430 & A0435)
|
Provider Name
|
Phone#
|
Location Address
|
Web site
|
|
Air Ambulance Specialists, Inc. dba AMR Air Ambulance
|
800-424-7060
|
8001 S Interport Blvd, #150, Englewood, CO 80112
|
www.AMRAirAmbulance.com
|
|
AeroCare Medical Transport Systems
|
630-466-0800
|
43W 752 Hwy 30, Sugar Gove, IL 60554
|
www.aerocare.com
|
|
Life Flight of Maine
|
888-421-4228
|
6 State St, Ste. 508, Bangor, Maine 04401
|
www.lifeflightmaine.org
|
|
Medway Air Ambulance, Inc.
|
800-233-0655
|
570 Briscoe Blvd, Lawrenceville, GA 30046
|
www.medwayair.com
|
|
Life Guard International, Inc. dba Flying ICU
|
702-740-5952
|
145 E. Reno Avenue Ste., E-7, Las Vegas, NV 89119
|
www.flyingicu.com
|
Rotary Wing (Helicopter) Providers (HCPCS Codes: A0431 and A0436)
|
Provider Name
|
Phone#
|
Location Address
|
Web site
|
|
LifeFlight of Maine
|
888-421-4228
|
6 State St, Ste. 508, Bangor, Maine 04401
|
www.lifeflightmaine.org
|
To arrange air transport originating outside the U.S., U.S. Virgin Islands and Puerto Rico, call 800-810-BLUE for BCBS Global Core formerly Bluecard Wordwide. We have identified an increasing trend in the billing of emergency room (ER) level 5 Evaluation and Management (E/M) codes. To help manage increasing healthcare costs, beginning August 1, 2019, we will initiate the post-pay review of professional ER claims billed with level 5 E/M Codes (99285 or G0384) to help ensure documentation meets or exceeds the components necessary to support its billing. Professional ER claims with the highest potential for up-coding will be selected.
We will request documentation for identified claims, and level 5 ER professional reviews will evaluate the appropriate use of the level 5 ER code based on the AMA CPT coding manuals, and Anthem guidelines. Reimbursement will be based on the ER E/M code the submitted documentation supports.
Please note, these coding reviews are not related to any prior notifications of reviews which examine the appropriate use of ERs for non-emergencies, nor do they include the examination of emergent versus non-emergent reasons patient utilize emergency room services.
In a continuation of our CRA reporting update articles throughout 2019, we request your assistance with respect to our Commercial Risk Adjustment (CRA) reporting processes.
As a reminder, there are two approaches that we take (retrospective and prospective) to improve risk adjustment reporting accuracy. We are focusing on performing appropriate interventions and chart reviews for patients with undocumented hierarchical condition categories (HCC), to close the documentation and coding gaps that we are seeing with our members enrolled in our Affordable Care Act (ACA) compliant plans.
This month we’d like to focus on the Prospective approach, and the request to our providers:
Anthem network providers -- usually primary care physicians -- may receive letters from our vendor, Inovalon, requesting that physicians:
- Schedule a comprehensive visit with patients identified to confirm or deny if previously coded or suspected diagnoses exists, and
- Submit a Health Assessment documenting the previously coded or suspected diagnoses (also called a SOAP Note -- Subjective, Objective, Assessment and Plan).
Incentives for properly submitted Health Assessments (in addition to the office visit reimbursement):
- $100 submitted electronically
- $50 submitted via fax
Health Assessment requests through Inovalon
We have engaged Inovalon -- an independent company that provides secure, clinical documentation services -- to help us comply with provisions of the ACA that require us to assess members’ relative health risk level. In the coming weeks and months, Inovalon will be sending letters to providers as part of our risk adjustment cycle, asking for their help with completing health assessments for some of our members.
This year will bring a new round of assessments. As a reminder, chronic conditions must be coded every year, and we encourage you to code to the greatest level of specificity on all Anthem claim submissions. If you have questions about the requests you receive, you can reach Inovalon directly at 866-682-6680.
Maximize your Incentive opportunity: submit electronically via Inovalon’s ePASS® tool
Join an ePASS webinar to learn how to submit a Health Assessment electronically and maximize your incentive opportunities. They are offered every Wednesday from 3:00 p.m. - 4:00 p.m. Register by sending an email to ePASSProviderRelations@inovalon.com with your name, organization, contact information and the date of the webinar you wish to attend.
- Teleconference: Dial 415-655-0002 (US Toll) and enter access code: 736 436 872
- WebEx: Visit https://inovalonmeet.webex.com and enter meeting number: 736 436 872
- Once you join the call, live support is available at any time by dialing *0
Alternative reporting engagement
ePASS is our preferred method for submission for the Prospective approach. However to improve engagement and collaborate with our Providers who are not submitting via ePASS, we have identified other alternatives which may be helpful and provide more flexibility with your current processes.
If you are interested in any of these alternative options, please contact Alicia Estrada, our CRA Network Education Representative, at Alicia.Estrada@anthem.com.
|
Alternative reporting option/Description
|
|
Availity Comprehensive Health Assessment
Availity will send a notification of members who have gaps and need assessments. The office will schedule members to be seen, at this time open gaps are displayed. Once the visit is completed, the office will complete the health assessment via Availity and the provider will review and sign off. Eligible for $100 incentive.
|
|
EPIC Patient Assessment Form (PAF)
Providers with EPIC as their EMR system can fax the EPIC PAF to Inovalon at 866-682-6680 without a coversheet. Eligible for $50 incentive.
|
|
Providers Existing Patient Assessment Form (PAF) -- Utilize providers existing EMR system and applicable PAF and fax to Inovalon at 866-682-6680. Must be submitted with a coversheet indicating "see attached Anthem Progress Note“. Eligible for $50 incentive.
Note: Please reach out to the CRA Network Education Representative listed above for confirmation that your EMR system’s PAF is compliant.
|
|
EPHC providers using PCMS -- Providers participating in our Enhanced Personal Health Care (EPHC) program can use member reports from our PCMS tool within Availity to schedule members for comprehensive visits. Providers use normal gap closure through claims submission. No Health Assessment needed.
|
|
List of members to be scheduled -- Anthem provides a member report for providers to schedule members for comprehensive visits. Providers use normal gap closure through claims submission. No Health Assessment needed.
|
|
Allscripts push notifications (combine with EMR Interoperability for Chart Requests from our Retrospective approach)
Once a member is scheduled for visit, provider will get notification of outstanding gaps. Benefit: Provider is aware upfront, at the time of the visit to address chronic conditions with members and code them accurately on their claim. No Health Assessment needed.
|
The Provider Manual will be updated for an effective date of July 1, 2019, and will be available on our website by May 1, 2019. To view the updated manual after May 1, go to anthem.com/provider > Find Resources for Your State > Select Maine > Provider Reference Materials/Provider Manuals > Provider Manual (effective 7/1/19).
In the March 2019 edition of our newsletter, Provider News, we announced the exciting updates we’ve made to the Medical Attachment submission tool. As you start using the updated medical attachment tool on the Availity Portal, you will see the following changes from the information we shared in March:
- File size – each attachment can be up to 10 MB with a maximum of 30 MB as the file size limit
- The addition of logos in your dashboard make it easy to quickly identify each payer
- The Medical Attachment tool will be retired from the Availity Portal soon, so we encourage you to start utilizing the ‘Attachment – New’ option now. We will provide an update in a future Provider News once the Medical Attachment tool retirement date is determined.
Other features of the updated medical attachment include:
- The ability to submit an itemized bill
- A different link titled “Attachment – New” where you will now submit medical records when Anthem has requested additional information to process a claim
- A new link on the attachment page called “Send Attachment” will allow you to start the process
- A record history of each entry provides you increased visibility of your submission
The Medical Attachment tool makes the process of submitting electronic documentation in support of a claim, simple and streamlined. You can use your tax identification number (TIN) or your NPI to register and submit solicited (requested by Anthem) medical record attachments through the Availity Portal.
Note: We will continue to keep you informed of upcoming changes to the ‘Attachment – New’ platform as we progress toward streamlining our electronic documentation functionality.
How to access/setup the solicited medical attachments tool for your office
Availity Administrators must complete these steps:
- From My Account Dashboard, select Enrollments Center > Medical Attachments Setup, follow the prompts and complete the following sections:
- Select Application > choose Medical Attachments Registration
- Provider Management > Select Organization from the drop-down. Add NPIs and/or tax IDs. (Multiples can be added separated by spaces or semi-colons.)
- Assign user access by checking the box in front of the user’s name. Users may be removed by unchecking their name.
Submitting medical attachments
Once the above setup is completed, Availity Users will complete these steps:
- Log in to www.availity.com.
- Select Claims and Payments > Attachments-New > Send Attachment Tab.
- Complete all required fields of the form.
- Attach supporting documentation.
- Submit.
Need training?
To access additional training for this Availity feature:
- Log in to the Availity Portal at www.availity.com.
- At the top of any Availity portal page, click Help and Training I Get Trained to open the Availity Learning Center (ALC) Catalog in a new browser tab. It is your dedicated ALC account.
- Search the Catalog using keyword Attachments to find training demo and on-demand courses.
- Select Enroll to register for a course and then go to your Dashboard to access it any time.
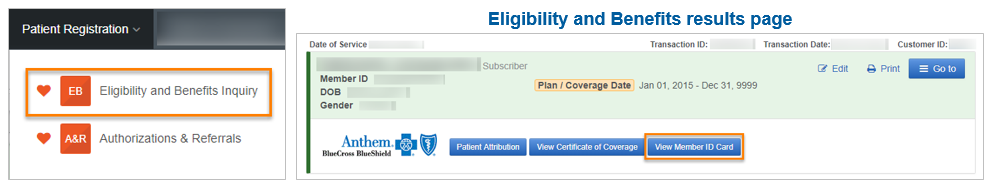
Have you had more Anthem members present with their ID card on their smartphone? We want to remind you of the ways you can access your own copy of their ID card.
In the October 2017 issue of Network Update, we informed you about our mobile app called Anthem Anywhere that allows members to manage their benefits on their smart phones, including the option of an electronic only version of their ID cards. We want to ensure a member’s electronic only ID card meets your needs.
Based on member requests and growing trends, we anticipate that by the year 2020, nearly 50% of our Local Plan members may choose the electronic ID card option, so we urge you to start using the available retrieval tools today.
Provider options for obtaining a copy of an electronic member ID card
- Online -- through the Availity Portal: Providers also have the option to view Anthem member ID cards online (and print if needed) from the Availity Portal at availity.com. When conducting an Eligibility and Benefits (E&B) Inquiry -- from the E&B Results page, select the blue button titled View Member ID Card. (Currently excludes BlueCard®, Federal Employee Program® (FEP) and some health plans’ Medicare Advantage and Medicaid members.)
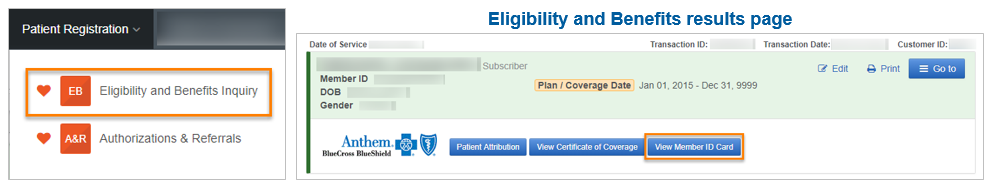
Note: As with all E&B Inquiries on Availity, providers must have the member ID number (including the three-character prefix) and one or more search options of date of birth, first name and last name.
- Email or Fax: Members can email/fax the card from his/her phone. When members are viewing their ID card on their phone, they will select the email or fax icon to forward their ID card.
These options are available for your patients who are members covered by our affiliated health plans in CA, CO, CT, GA, IN, KY, ME, MO, NH, NV, NY, OH, WI and VA.
Members are still required to have a copy of their card in one format or another, whether hard copy or electronic, in order for services to be rendered. See our Quick Reference Guide for further details.
Quick Reference Guide
See our Electronic Member ID Cards – Quick Reference Guide for more details and information on:
- Frequently Asked Questions
- Details on provider options for obtaining a copy of an electronic member ID card
- Sample electronic member ID cards
Effective August 1, 2019, we will upgrade to the 23rd edition of MCG care guidelines for the following modules: Inpatient & Surgical Care (ISC), General Recovery Care (GRC), Chronic Care (CC), Recovery Facility Care (RFC), Behavioral Health Care (BHC).
Goal Length of Stay (GLOS) changes for Inpatient & Surgical Care (ISC)
|
Guideline
|
MCG Number
|
23rd Edition GLOS
|
22nd Edition GLOS
|
|
Neurology-Traumatic Brain Injury, Nonsurgical Treatment
|
M-78
|
Ambulatory or 2 days
|
2 days
|
|
Orthopedics-Lumbar Fusion
|
S-820
|
2 days postoperative
|
3 days postoperative
|
New Optimal Recovery Guidelines (ORGs), Common Complications and Conditions (CCC) and Level of Care (LOC) Guidelines
|
Module
|
Guideline
|
Title
|
MCG Number
|
|
ISC
|
ORG
|
Anorexia Nervosa, Child or Adolescent
|
P-585
|
|
ISC
|
ORG
|
Substance-Related Disorders, Child or Adolescent
|
P-596
|
|
ISC
|
ORG
|
Left Atrial Appendage Closure, Percutaneous
|
M-333
|
|
ISC
|
ORG
|
Abdominal Pain, Undiagnosed, Pediatric
|
P-05
|
|
ISC
|
ORG
|
Craniotomy for Traumatic Brain Injury or Intracerebral Hemorrhage, Pediatric
|
P-414
|
|
ISC
|
ORG
|
Craniotomy, Supratentorial, Pediatric
|
P-411
|
|
ISC
|
ORG
|
Headaches, Pediatric
|
P-185
|
|
ISC
|
ORG
|
Hernia Repair (Non-Hiatal), Pediatric
|
P-1305
|
|
ISC
|
ORG
|
Inflammatory Bowel Disease, Pediatric
|
P-565
|
|
ISC
|
ORG
|
Pelvic Inflammatory Disease (PID), Acute, Pediatric
|
P-260
|
|
ISC
|
ORG
|
Spine, Scoliosis, Posterior Instrumentation, Pediatric
|
P-1056
|
|
ISC
|
ORG
|
Supraventricular Arrhythmias, Pediatric
|
P-510
|
|
ISC
|
CCC
|
Pain: Common Complications and Conditions
|
CCC-050
|
|
RFC
|
ORG
|
Degenerative Joint Disease (DJD)
|
M-7030
|
|
BHC
|
LOC
|
Obsessive-Compulsive and Related Disorders, Adult: Inpatient Care
|
B-030-IP
|
|
BHC
|
LOC
|
Obsessive-Compulsive and Related Disorders, Child or Adolescent: Inpatient Care
|
B-029-IP
|
|
BHC
|
LOC
|
Obsessive-Compulsive and Related Disorders: Residential Care
|
B-030-RES
|
|
BHC
|
LOC
|
Obsessive-Compulsive and Related Disorders: Partial Hospital Program
|
B-030-PHP
|
|
BHC
|
LOC
|
Obsessive-Compulsive and Related Disorders: Intensive Outpatient Program
|
B-030-IOP
|
|
BHC
|
LOC
|
Obsessive-Compulsive and Related Disorders: Acute Outpatient Care
|
B-030-AOP
|
Anthem Customizations to MCG care guideline 23rd Edition
Effective August 1, 2019, the following MCG care guideline 23rd edition customizations will be implemented.
- Left Atrial Appendage Closure, Percutaneous (W0157) - customized to refer to SURG.00032 Transcatheter Closure of Patent Foramen Ovale and Left Atrial Appendage for Stroke Prevention
- Spine, Scoliosis, Posterior Instrumentation, Pediatric (W0156) - customized to refer to Musculoskeletal Program Clinical Appropriateness Guidelines, Level of Care Guidelines and Preoperative Admission Guidelines
To see a more detailed summary of customizations, visit our website.
For questions, please contact the provider service number on the back of the member's ID card. The following new and revised medical policies were endorsed at the January 24, 2019 Medical Policy & Technology Assessment Committee (MPTAC) meeting. These, and all Anthem medical policies, are available at anthem.com/provider > scroll down and select ‘Find Resources for [state]’ > Medical Policies and Clinical UM Guidelines.
If you do not have access to the internet, you may request a hard copy of any updated policy by contacting the Provider Call Center.
Revised Clinical Guidelines effective January 31, 2019
(The following adopted guidelines were revised to expand medical necessity indications or criteria)
- CG-DRUG-50 - Paclitaxel, protein-bound (Abraxane®)
- CG-DRUG-99 - Elotuzumab (Empliciti™)
- CG-SURG-27 - Sex Reassignment Surgery
- CG-SURG-83 - Bariatric Surgery and Other Treatments for Clinically Severe Obesity
Revised Clinical Guidelines effective February 27, 2019
(The following adopted guidelines were revised to expand medical necessity indications or criteria.)
- CG-SURG-77 - Refractive Surgery
- CG-DRUG-106 - Brentuximab Vedotin (Adcetris®)
Revised Clinical Guidelines effective February 27, 2019
(The following adopted guidelines were reviewed and had no significant changes to the policy position or criteria.)
- CG-ANC-04 - Ambulance Services; Air and Water
- CG-BEH-14 - Intensive In-Home Behavioral Health Services
- CG-BEH-15 - Activity Therapy for Autism Spectrum Disorders and Rett Syndrome
- CG-DME-10 - Durable Medical Equipment
- CG-DME-31 - Wheeled Mobility Devices: Wheelchairs - Powered, Motorized, with or without Power Seating Systems, and Power Operated Vehicles (POVs)
- CG-DME-33 - Wheeled Mobility Devices: Manual Wheelchairs - Ultra Lightweight
- CG-DME-43 - Oscillatory Devices for Airway Clearance (High Frequency Chest Compression)
- CG-DRUG-01 - Off-Label Drug and Approved Orphan Drug Use
- CG-DRUG-28 - Alglucosidase alfa (Lumizyme®)
- CG-DRUG-29 - Hyaluronan Injections
- CG-DRUG-43 - Natalizumab (Tysabri®)
- CG-DRUG-82 - Prostacyclin Infusion Therapy and Inhalation Therapy for Treatment of Pulmonary Arterial Hypertension
- CG-DRUG-83 - Growth Hormone
- CG-DRUG-84 - Belimumab (Benlysta®)
- CG-DRUG-85 - Tesamorelin (Egrifta®)
- CG-DURG-86 - Ocriplasmin (Jetrea®) Intravitreal Injection Treatment
- CG-DRUG-93 - Sarilumab (Kevzara®)
- CG-LAB-13 - Skin Nerve Fiber Density Testing
- CG-MED-23 - Home Health
- CG-MED-38 - Inpatient Admission for Radiation Therapy for Cervical or Thyroid Cancer
- CG-MED-39 - Central (Hip or Spine) Bone Density Measurement and Screening for Vertebral Fractures Using Dual Energy X-Ray Absorptiometry
- CG-OR.PR-05 - Myoelectric Upper Extremity Prosthetic Devices
- CG-SURG-03 - Blepharoplasty, Blepharoptosis Repair, and Brow Lift
- CG-SURG-70 - Gastric Electrical Stimulation
- CG-SURG-71 - Reduction Mammoplasty
- CG-SURG-72 - Endothelial Keratoplasty
- CG-SURG-75 - Transanal Endoscopic Microsurgical (TEM) Excision of Rectal Lesions
- CG-THER-RAD-07 - Intravascular Brachytherapy (Coronary and Noncoronary)
Adopted Clinical Guidelines effective March 21, 2019
(The following guidelines were previously medical policies and have been adopted with no significant changes.)
- CG-SURG-94 - Keratoprosthesis (was SURG.00115)
- CG-SURG-95 - Sacral Nerve Stimulation (SNS) and Percutaneous Tibial Nerve Stimulation (PTNS) for Urinary and Fecal Incontinence; Urinary Retention (was SURG.00117)
- CG-SURG-96 - Intraocular Telescope (was SURG.00136)
Revised Clinical Guidelines effective August 1, 2019
(The following adopted guidelines were revised and might result in services that were previously covered but may now be found to be not medically necessary.)
- CG-DRUG-106 - Brentuximab Vedotin (Adcetris®)
- CG-MED-73 - Hyperbaric Oxygen Therapy (Systemic/Topical)
- CG-SURG-27 - Sex Reassignment Surgery
The following new and revised medical policies were endorsed at the January 24, 2019 Medical Policy & Technology Assessment Committee (MPTAC) meeting. These, and all Anthem medical policies, are available at anthem.com/provider > scroll down and select ‘Find Resources for [state]’ > Medical Policies and Clinical UM Guidelines.
If you do not have access to the internet, you may request a hard copy of any updated policy by contacting the Provider Call Center.
Please note that the Federal Employee Program® Medical Policy Manual may be accessed at www.fepblue.org > Benefit Plans > Brochures and Forms > Medical Policies.
Revised Medical Policies effective January 31, 2019
(The following policies were revised to expand medical necessity indications or criteria.)
- DRUG.00071 - Pembrolizumab (Keytruda®)
- DRUG.00088 - Atezolizumab (Tecentriq®)
- OR-PR.00003 - Microprocessor Controlled Lower Limb Prostheses
Revised Medical Policies effective February 27, 2019
(The following policies were revised to expand medical necessity indications or criteria.)
- SURG.00011 - Allogeneic, Xenographic, Synthetic and Composite Products for Wound Healing and Soft Tissue Grafting
- TRANS.00035 - Mesenchymal Stem Cell Therapy for the Treatment of Joint and Ligament Disorders, Autoimmune, Inflammatory and Degenerative Diseases
Revised Medical Policies effective February 27, 2019
(The following policies were reviewed and had no significant changes to the policy position or criteria.)
- ANC.00009 - Cosmetic and Reconstructive Services of the Trunk and Groin
- DME.00025 - Self-Operated Spinal Unloading Devices
- DRUG.00013 - Administration of Immunoglobulin as a Treatment of Recurrent Spontaneous Abortion
- DRUG.00027 - Ziconotide Intrathecal Infusion (Prialt®) for Severe Chronic Pain
- DRUG.00078 - Proprotein Convertase Subtilisin Kexin 9 (PCSK9) Inhibitors
- DRUG.00080 - Monoclonal Antibodies for the Treatment of Eosinophilic Conditions
- DRUG.00081 - Eteplirsen (Exondys 51®)
- DRUG.00082 - Daratumumab (DARZALEX®)
- GENE.00010 - Genotype Testing for Genetic Polymorphisms to Determine Drug-Metabolizer Status
- GENE.00016 - Gene Expression Profiling for Colorectal Cancer
- GENE.00034 - SensiGene™ Fetal RHD genotyping
- GENE.00036 - Genetic Testing for Hereditary Pancreatitis
- GENE.00037 - Genetic Testing for Macular Degeneration
- GENE.00039 - Genetic Testing for Frontotemporal Dementia
- GENE.00046 - Prothrombin G20210A (Factor II) Mutation Testing
- LAB.00024 - Immune Cell Function Assay
- LAB.00034 - Serological Antibody Testing for Helicobacter Pylori
- MED.00002 - Selected Sleep Testing Services
- MED.00007 - Prolotherapy for Joint and Ligamentous Conditions
- MED.00013 - Parenteral Antibiotics for the Treatment of Lyme Disease
- MED.00065 - Hepatic Activation Therapy
- MED.00074 - Computer Analysis and Probability Assessment of Electrocardiographic-Derived Data
- MED.00091 - Rhinophototherapy
- MED.00092 - Automated Nerve Conduction Testing
- MED.00097 - Neural Therapy
- MED.00115 - Outpatient Cardiac Hemodynamic Monitoring Using a Wireless Sensor for Heart Failure Management
- MED.00116 - Near-Infrared Spectroscopy Brain Screening for Hematoma Detection
- MED.00117 - Autologous Cell Therapy for the Treatment of Damaged Myocardium
- MED.00122 - Wilderness Programs
- RAD.00012 - Ultrasound for the Evaluation of the Paranasal Sinuses
- RAD.00053 - Cervical and Thoracic Discography
- REHAB.00003 - Hippotherapy
- SURG.00007 - Vagus Nerve Stimulation
- SURG.00036 - Fetal Surgery for Prenatally Diagnosed Malformations
- SURG.00047 - Transendoscopic Therapy for Gastroesophageal Reflux Disease and Dysphagia
- SURG.00073 - Epiduroscopy
- SURG.00079 - Nasal Valve Suspension
- SURG.00097 - Vertebral Body Stapling for the Treatment of Scoliosis in Children and Adolescents
- SURG.00099 - Convection Enhanced Delivery of Therapeutic Agents to the Brain
- SURG.00100 - Cryoablation for Plantar Fasciitis and Plantar Fibroma
- SURG.00102 - Artificial Anal Sphincter for the Treatment of Severe Fecal Incontinence
- SURG.00106 - Ablative Techniques as a Treatment for Barrett’s Esophagus
- SURG.00111 - Axial Lumbar Interbody Fusion
- SURG.00112 - Occipital Nerve and Supraorbital Nerve Stimulation
- SURG.00122 - Venous Angioplasty with or without Stent Placement or Venous Stenting Alone
- SURG.00123 - Transmyocardial/ perventricular Device Closure of a Ventricular Septal Defect
- SURG.00138 - Laser Treatment of Onychomycosis
- SURG.00146 - Extracorporeal Carbon Dioxide Removal
- THER-RAD.00008 - Neutron Beam Radiotherapy
- THER-RAD.00009 - Intraocular Epiretinal Brachytherapy
- TRANS.00004 - Cell Transplantation (Adrenal-Brain, Fetal Mesencephalic, and Fetal Xenograft)
- TRANS.00008 - Liver Transplant
- TRANS.00009 - Lung and Lobar Transplant
- TRANS.00010 - Autologous and Allogenic Pancreatic Islet Cell Transplant
- TRANS.00026 - Heart-Lung Transplantation
- TRANS.00033 - Heart Transplant
Archived Medical Policies effective March 21, 2019
(The following policies have been archived and their content has been transferred to new Clinical UM Guidelines.)
- SURG.00115 – Keratoprosthesis (Recategorized to CG-SURG-94)
- SURG.00117 - Sacral Nerve Stimulation (SNS) and Percutaneous Tibial Nerve Stimulation (PTNS) for Urinary and Fecal Incontinence; Urinary Retention (Recategorized to CG-SURG-95)
- SURG.00136 - Intraocular Telescope (Recategorized to CG-SURG-96)
Revised Medical Policy effective August 1, 2019
(The following policy was revised to expand medical necessity indications or criteria.)
- TRANS.00035 - Mesenchymal Stem Cell Therapy for the Treatment of Joint and Ligament Disorders, Autoimmune, Inflammatory and Degenerative Diseases
Revised Medical Policies effective August 1, 2019
(The policies below were revised and might result in services that were previously covered but may now be found to be either not medically necessary and/or investigational.)
- MED.00110 - Growth Factors, Silver-based Products and Autologous Tissues for Wound Treatment and Soft Tissue Grafting
- SURG.00037 - Treatment of Varicose Veins (Lower Extremity)
New Medical Policy effective August 1, 2019
(The policy below was created and might result in services that were previously covered but may now be found to be either not medically necessary and/or investigational.)
- LAB.00036 - Multiplex Autoantigen Microarray Testing for Diagnosing Systemic Lupus Erythematosus
Beginning with dates of service on or after April 28, 2019, our policy language will be updated to allow the lower level definitive code drug testing of 1-7 drug class(es) (G0480) on the same day as presumptive services. Additionally, the definitive drug testing related coding section was expanded for clarification. For more information about this policy, visit the Reimbursement Policy page at anthem.com/provider. In the February edition of our provider newsletter, Provider News, we shared that the following clinical criteria will be effective May 1, 2019. We will begin the medical step therapy review process for non-oncology uses of these drugs at this time. We will notify you when we begin the medical step therapy review process for oncology indications.
Colony Stimulating Factor Agents ING-CC-0002
Effective for dates of service on and after May 1, 2019, the following specialty pharmacy codes from new or current criteria will be included in our existing specialty pharmacy medical step therapy review process. Zarxio® will be the preferred short-acting colony stimulating factor (CSF) agent over Neupogen®, Granix®, and Nivestym™®.
Pre-service clinical review of these specialty pharmacy drugs will be managed by AIM Specialty Health® (AIM), a separate company.
Additional information regarding biosimilar drugs can be found by viewing the attached reference document, “Biosimilar Drugs – What are they?”.
To access the clinical criteria information please click here.
|
Clinical Criteria
|
Status
|
Drug
|
HCPCS or CPT Code
|
NDC Code
|
|
ING-CC-0002
|
Preferred Agent
|
Zarxio®
|
Q5101
|
61314-0304-01
61314-0304-10
61314-0312-01
61314-0312-10
61314-0318-01
61314-0318-10
61314-0326-01
61314-0326-10
|
|
ING-CC-0002
|
Non-Preferred Agent
|
Neupogen®
|
J1442
|
55513-0530-01
55513-0530-10
55513-0546-01
55513-0546-10
55513-0924-01
55513-0924-10
55513-0924-91
55513-0209-01
55513-0209-10
55513-0209-91
|
|
ING-CC-0002
|
Non-Preferred Agent
|
Granix®
|
J1447
|
63459-0910-11
63459-0910-12
63459-0910-15
63459-0910-17
63459-0910-36
63459-0912-11
63459-0912-12
63459-0912-15
63459-0912-17
63459-0912-36
|
|
ING-CC-0002
|
Non-Preferred Agent
|
Nivestym™
|
Q5110
|
00069-0291-10
00069-0291-01
00069-0292-01
00069-0292-10
|
For more information on copayment/coinsurance requirements and their applicable drug classes, drug lists and changes, prior authorization criteria, procedures for generic substitution, therapeutic interchange, step therapy or other management methods subject to prescribing decisions and other requirements, restrictions or limitations that apply to certain drugs, visit anthem.com/pharmacyinformation.
- To locate the commercial drug list, select ‘Click here to access your drug list’.
- To locate the Marketplace Select Formulary and pharmacy information, scroll down to ‘Select Drug Lists’, then select the applicable state’s drug list link.
The commercial and marketplace drug lists are reviewed and updates are posted to the website quarterly (the first of the month for January, April, July and October).
Federal Employee Program (FEP) pharmacy updates and other pharmacy related information may be accessed at www.fepblue.org > Pharmacy Benefits. This drug list is also reviewed and updated regularly as needed. Agents for Hereditary Angioedema ING-CC-0034
Effective for dates of service on and after August 1, 2019, the following specialty pharmacy codes from new or current clinical criteria will be included in our existing specialty pharmacy medical step therapy review process. Haegarda® and Takhzyro™ will be the preferred prophylactic agents over Cinryze®.
Please note, inclusion of NDC code on your claim will help expedite claim processing of drugs billed with a Not Otherwise Classified (NOC) code.
To access the clinical criteria information please click here.
|
Clinical Criteria
|
Status
|
Drug
|
HCPCS or CPT Code
|
NDC Code
|
|
ING-CC-0034
|
Preferred Agent
|
Haegarda®
|
J0599
|
63833-0828-02
63833-0829-02
|
|
ING-CC-0034
|
Preferred Agent
|
Takhzyro™
|
J3490, J3590, C9399
|
47783-0644-01
|
|
ING-CC-0034
|
Non-Preferred Agent
|
Cinryze®
|
J0598
|
42227-0081-05
|
Anthem Medicare Advantage plans follow original Medicare guidelines and billing requirements for partial hospitalization services. CMS regulations (42 CFR 410.43(c)(1)) state that partial hospitalization programs (PHPs) are intended for members who require a minimum of 20 hours per week of therapeutic services as evidenced in their plan of care. All partial hospitalization services require prior authorization. The full article is located online.
In 2019, Anthem will work with Optum Health, using their copy partner CiOX, to request medical records with dates of service for the target year 2018, through present day, then review and code the record. Read the full article online.
Each year, falls result in more than 2.8 million ER visits, 800,000 hospitalizations and 27,000 deaths. Additional information about helping patients enrolled in Medicare Advantage prevent falls is available on our website.
The State of Maine Health Plan provides benefits for a blood pressure cuff, CPT A4670. When obtained from an in-network supplier, the claim will process at 100% of the maximum allowable amount (MAA) with no member cost shares. When obtained from an out of network supplier, the member will be responsible for their out of network cost sharing, plus balance billing (amounts above the MAA).
Please refer to our Find a Doctor tool to find an in-network supplier.
Note: A prescription is required for purchase. |