Provider News MaineDecember 1, 2019 December 2019 Anthem Maine Provider NewsAdministrativeAdministrative | Anthem Blue Cross and Blue Shield | Commercial | November 30, 2019 Coordination of careState & FederalState & Federal | Anthem Blue Cross and Blue Shield | Medicare Advantage | November 30, 2019 Group Retiree PPO plans
Beginning with dates of service on or after December 1, 2019, our current Durable Medical Equipment policy will be retired and will be replaced by the new Durable Medical Equipment – Rent to Purchase policy and the new Durable Medical Equipment - Modifiers policy. The new Durable Medical Equipment – Rent to Purchase policy has the same reimbursement guidelines and requirements as the current Durable Medical Equipment policy. The new Durable Medical Equipment - Modifiers policy has the same reimbursement guidelines for DME Modifiers as the current Durable Medical Equipment policy.
For more information about these new policies, visit the reimbursement policy page at anthem.com. The delivery of quality health care requires cooperation between patients, their providers and their health care benefit plans. One of the first steps is for patients and providers to understand their rights and responsibilities. Therefore, in line with our commitment to involve the health plan, participating practitioners and members in our system, we have adopted a Members’ Rights and Responsibilities statement.
It can be found on our website at anthem.com/provider > select state> scroll down and select ‘Find Resources for [state], then Health & Wellness > Quality Improvement Standards > Member Rights & Responsibilities. Practitioners may access the FEP member portal at www.fepblue.org/memberrights to view the FEPDO Member Rights Statement. Our utilization management (UM) decisions are based on the appropriateness of care and service needed, as well as the member’s coverage according to their health plan. We do not reward providers or other individuals for issuing denials of coverage, service or care. Nor do we make decisions about hiring, promoting, or terminating these individuals based on the idea or thought that they will deny benefits. In addition, we do not offer financial incentives for UM decision makers to encourage decisions resulting in under-utilization. Our medical policies are available on our website at anthem.com/provider > Provider Resources > Policies and Guidelines > select state > View Medical Policies & UM Guidelines.
You can also request a free copy of our UM criteria from our medical management department, and providers may discuss a UM denial decision with a physician reviewer by calling us at the toll-free numbers listed below. UM criteria are also available on our website at anthem.com/provider > Provider Resources > Policies and Guidelines > select state > View Medical Policies & UM Guidelines.
We work with providers to answer questions about the utilization management process and the authorization of care. Here’s how the process works:
- Call us toll free from 8:30 a.m. – 5:00 p.m. Monday through Friday (except on holidays). More hours may be available in your area. Federal Employee Program hours are 8:00 a.m. – 7 p.m.
- If you call after normal business hours, you can leave a private message with your contact information. Our staff will return your call on the next business day. Calls received after midnight will be returned the same business day.
- Our associates will contact you about your UM inquiries during business hours, unless otherwise agreed upon.
The following phone numbers are for physicians and their staffs only. Members should call the customer service number on their health plan ID card.
|
To Discuss UM Process
and Authorizations
|
To Discuss Peer-to-Peer UM Denials w/Physicians
|
To Request UM Criteria
|
TDD/TTY
|
|
800-392-1016
Transplant:
800-255-0881
Behavioral Health:
800-755-0851
Autism:
844-269-0538
FEP
Phone: 800-860-2156
Fax: 800-732-8318 (UM)
Fax: 877-606-3807 (ABD)
|
800-437-7162
FEP
800-860-2156
|
800-437-7162
FEP
Phone: 800-860-2156
Fax: 800-732-8318 (UM)
Fax: 877-606-3807 (ABD)
|
711,
Or
TTY: 800-437-1220
Voice: 800-457-1220
|
For language assistance, members can simply call the Customer Service phone number on the back of their ID cards and a representative will be able to assist them.
Our utilization management associates identify themselves to all callers by first name, title and our company name when making or returning calls. They can inform you about specific utilization management requirements, operational review procedures, and discuss utilization management decisions with you. Coordination of care among providers is a vital aspect of good treatment planning to help ensure appropriate diagnosis, treatment and referral. We would like to take this opportunity to stress the importance of communicating with your patient’s other health care practitioners. This includes primary care physicians (PCPs) and medical specialists, as well as behavioral health practitioners.
Coordination of care is especially important for patients with high utilization of general medical services and those referred to a behavioral health specialist by another health care practitioner. We urge all practitioners to obtain the appropriate permission from these patients to coordinate care between behavioral health and other health care practitioners at the time treatment begins.
We expect all health care practitioners to:
- Discuss with the patient the importance of communicating with other treating practitioners.
- Obtain a signed release from the patient and file a copy in the medical record.
- Document in the medical record if the patient refuses to sign a release.
- Document in the medical record if you request a consultation.
- If you make a referral, transmit necessary information; if you are furnishing a referral, report appropriate information back to the referring practitioner.
- Document evidence of clinical feedback (i.e., consultation report) that includes, but is not limited to:
- Diagnosis
- Treatment plan
- Referrals
- Psychopharmacological medication (as applicable)
In an effort to facilitate coordination of care, we have several tools available on our provider website including a Coordination of Care Form and Coordination of Care Letter Templates for both behavioral health and other medical practitioners. Behavioral health tools include forms, brochures and screening tools for substance abuse, ADHD and autism. Please refer to our website for a complete list. These forms, template letters and behavioral health tools are available at www.anthem.com/provider/forms/.
Managing illness can sometimes be a difficult thing to do. Knowing whom to contact, understanding test results or how to get needed resources can be a bigger piece of a healthcare puzzle that for some, are frightening and complex issues to handle.
We are available to offer assistance in these difficult moments with our Case Management Program. Our case managers are part of an interdisciplinary team of clinicians and other resource professionals who are there to support members, families, primary care physicians and caregivers. The case management process utilizes experience and expertise of the care coordination team whose goal is to educate and empower our members to increase self-management skills, understand their illness, and learn about care choices in order to access quality, efficient health care.
Members or caregivers can refer themselves or family members by calling the number located in the grid below. They will be transferred to a team member based on the immediate need. Physicians can also refer by contacting us telephonically or through electronic means. No issue is too big or too small. We can help with transitions across level of care so that members and caregivers are better prepared and informed about healthcare decisions and goals.
Case management contact information:
|
Email Address (if available)
|
Telephone
|
Business Hours
|
|
CMReferralSpecialistNE@anthem.com
|
800-231-8254
Federal Employee Program® (FEP®):
800-711-2225
|
Mon. - Fri., 8:00 am - 7:00 pm
FEP: 8:00 am - 7:00 pm
|
As part of our commitment to provide you with the latest clinical information and educational materials, we have adopted nationally recognized medical, behavioral health and preventive health guidelines, which are available to providers on our website. The guidelines, which are used for our Quality programs, are based on reasonable, medical evidence, and are reviewed for content accuracy, current primary sources, the newest technological advances and recent medical research.
All guidelines are reviewed annually, and updated as needed. The current guidelines are available on our website at anthem.com/provider > scroll down and select ‘Find Resources for [state]’ > Health and Wellness > Practice Guidelines. We continue to support cost transparency, which involves making provider cost information available to members. We do this via our consumer transparency tools, BCBS AXIS/NCCT Cost Comparison, Care and Cost Finder, and Castlight. We display costs for common procedures that are non-emergent, high-cost, or high-volume. For these procedures, Anthem derives a cost range for the total episode of care, which includes all facility, professional, and ancillary services provided during an admission or outpatient visit. These costs are based on historical rates.
Cost and quality information is available nationally through the Blue Cross and Blue Shield Association and is known as the National Consumer Cost Tool (NCCT). In addition, the BCBS AXIS/NCCT data are used as the basis for the Care and Cost Finder tool and other third party transparency initiatives, which can be found on the home page of Anthem's Consumer Portal website.
Anthem has expanded the cost information that will be available to members through the Care and Cost Finder tool. Members using Care and Cost Finder will be able to view provider-specific costs for additional professional and ancillary services, including provider-specific office visit cost data.
The current version of the cost comparison transparency data will be updated in January 2020, and will be available for provider review in December 2019 prior to its release via Availity. If you have questions regarding Anthem Care Comparison, Estimate Your Cost, or our expanded transparency initiatives, please contact David Spencer, Sr. Provider Network Manager at david.spencer@anthem.com. Maintaining accurate provider information is critically important to ensure our members have timely and accurate access to care.
Additionally, we are required by Centers for Medicare & Medicaid Services (CMS) to include accurate information in provider directories for certain key provider data elements. For Anthem to remain compliant with federal and state requirements, providers must communicate changes to us 30 days in advance of a change or as soon as possible.
Key data elements
The data elements required by CMS and crucial for member access to care are:
- Physician name
- Location (such as address, suite if appropriate, city/state, zip code)
- Phone number
- Accepting new patient status
- Hospital affiliations
- Medical group affiliations
We are also encouraged (and in some cases required by regulatory/accrediting entities) to include accurate information for the following provider data elements:
- Physician gender
- Languages spoken
- Office hours
- Provider specialty/specialties
- Physical disabilities accommodations
- Indian Health Service status
- Licensing information (i.e., medical license number, license state, National Provider Identifier - NPI)
- Email and website address
How to verify and update your information
To verify information, go to anthem.com, select ‘Providers’, then under ‘Provider Resources’ select ‘Find a Doctor’ tool. Use ‘Search as a Guest’ at the bottom. If your information is not correct, please update the information as soon as possible.
To update information, go to anthem.com, select “Providers’, and then under ‘Provider Resources’ select ‘Provider Maintenance’ and follow the online prompts. In our ongoing efforts to streamline and simplify our payment recovery process, we will be consolidating our National Accounts membership to a central system. This consolidation will align the payment recovery processes to be the same as the majority of our other lines of business.
Our recovery process for National Accounts membership is reflected on the electronic remittance advice (835) in the PLB segment. The requested recovered amount on the electronic remittance advice (835) is displayed at the time of the recovery.
As National Accounts membership transitions and claims are adjusted for recovery on the central system, the requested recovered amount will be held for 49 days. This will allow ample time for you to review the requests, dispute the requests and/or send in a check payment. During this time, the negative balances due are reflected on paper remits only within the “Deferred Negative Balance” section.
After 49 days, the requested recovered amount is reflected on the electronic remittance advice (835) in the PLB segment.
If you have any questions or concerns, please contact the E-Solutions Service Desk toll free at 800-470-9630. As a reminder, we will update our claim editing software monthly throughout 2020 with the most common updates occurring quarterly in February, May, August and November of 2020. These updates will:
- reflect the addition of new, and revised codes (e.g. CPT, HCPCS, ICD-10, modifiers) and their associated edits
- include updates to National Correct Coding Initiative (NCCI) edits
- include updates to incidental, mutually exclusive, and unbundled (rebundle) edits
- include assistant surgeon eligibility in accordance with the policy
- include edits associated with reimbursement policies including, but not limited to, frequency edits, medically unlikely edits, bundled services and global surgery preoperative and post-operative periods assigned by The Centers for Medicare & Medicaid Services (CMS)
- apply to any provider or provider group (tax identification number) and may apply to both institutional and professional claim types
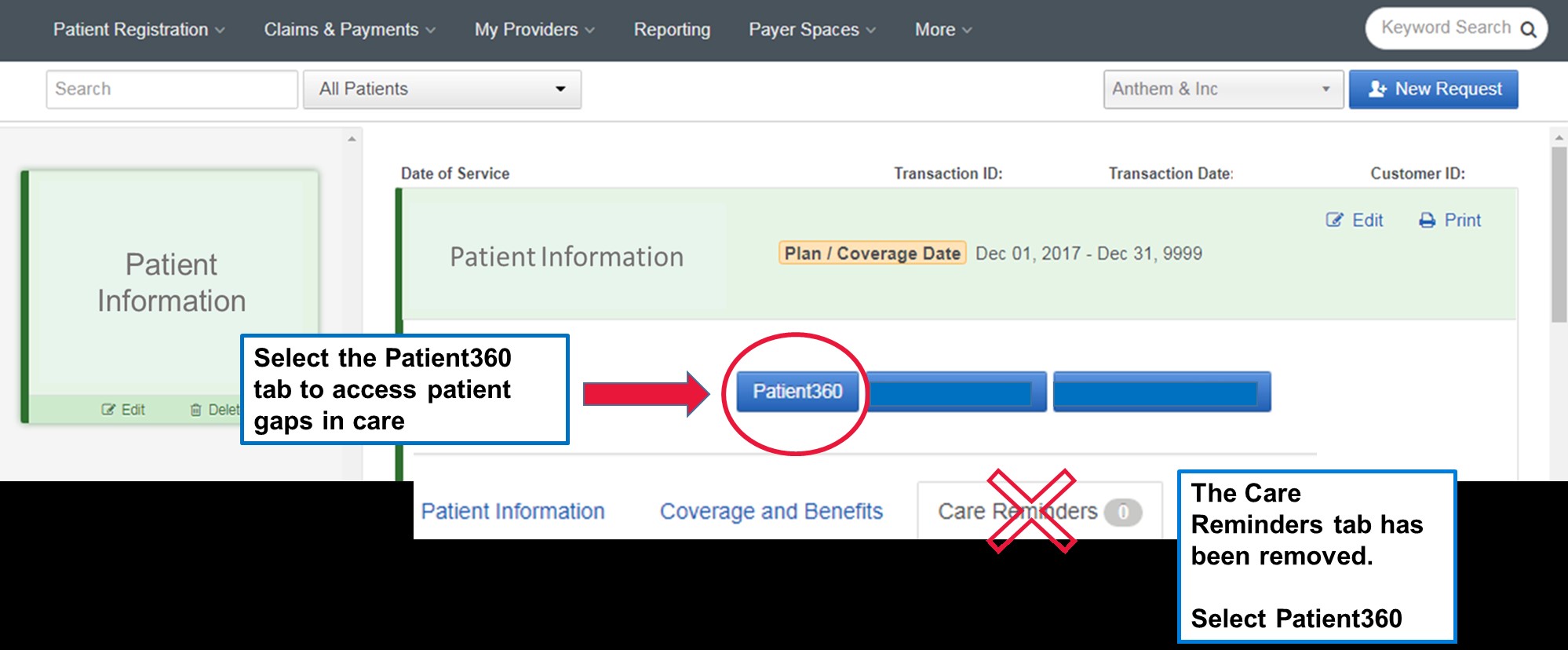
Patient360 is a longitudinal patient record (LPR) where you can access the complete view of Anthem information associated with an Anthem member.
You may have noticed that the Care Reminders tab on your Anthem patient’s Eligibility and Benefits return on Availity was recently removed. You can still retrieve these important patient gaps in care through Patient360.
You are required to have the Patient360 role assigned to you by your Availity administrator to see the Patient360 tab located at the top of the patient’s Eligibility and Benefits return. To access Patient360 select the tab and follow the steps to open the application.
If your patient does have a gap in care, you will see the red alert button on the top of Patient360 Member Care Summary. Details of the care gap can be found in the Active Alerts section.
Availity Eligibility and Benefits: Patient360 access
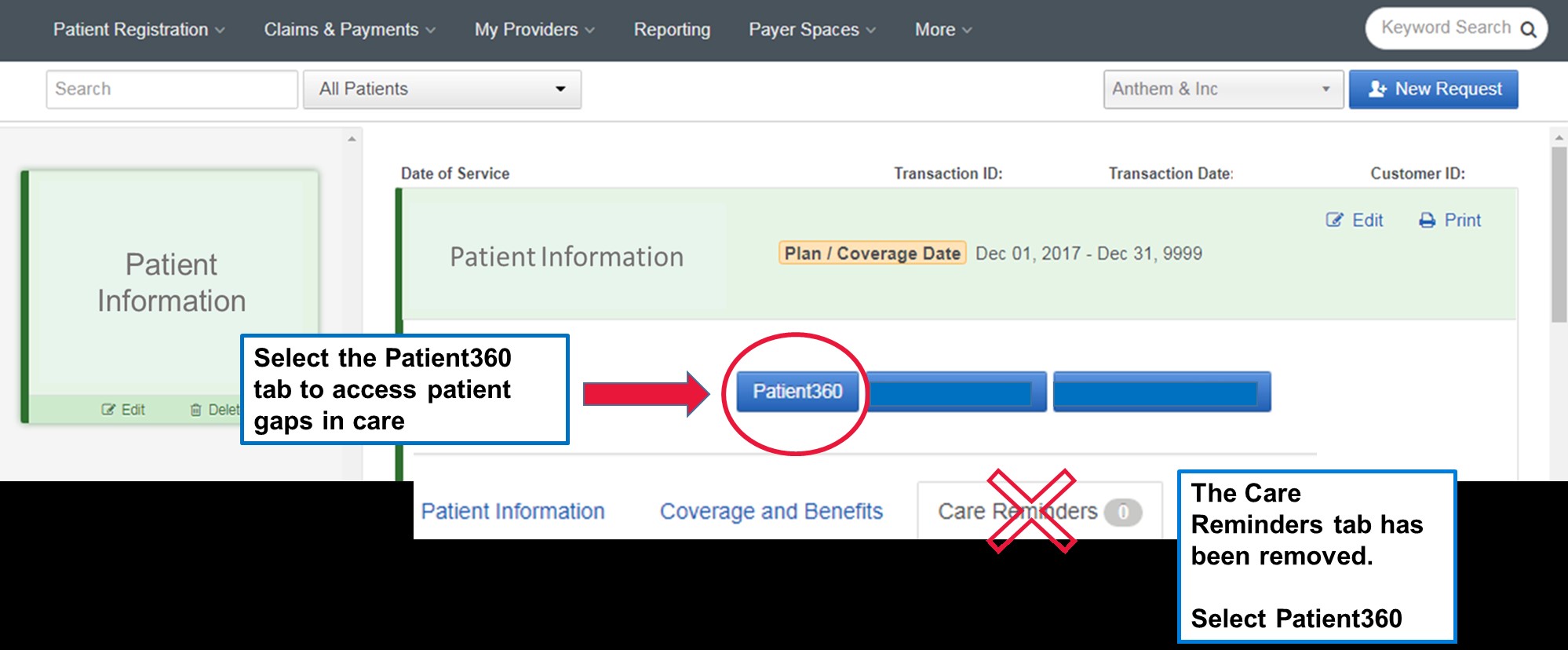
Patient360 Active Alerts located on the Member Care Summary

On January 1, 2019, a change to CPT codes for psychological and neuropsychological test administration and evaluation services was released. The new codes did not crosswalk on a one-to-one basis with the deleted codes. The coding changes separated test administration from test evaluation, psychological testing from neuropsychological testing, and defined the testing performed by a professional or technician. As a reminder, the new codes were as follows:
Neurobehavioral status exams are clinical interview examinations performed by a psychologist or neuropsychologist to assess thinking, reasoning and judgment. Providers should continue to use CPT code 96116 when billing for the first hour and new code 96121 when billing for each additional hour.
Testing evaluation services include the selection of the appropriate tests to be administered; integration of patient data; interpretation of standardized test results and clinical data; clinical decision-making; treatment planning; and reporting and interactive feedback to the patient, family members, or caregivers, when performed. Providers should now use CPT code 96130 to bill for the first hour of psychological testing evaluation services and 96131 for each additional hour. Neuropsychological evaluation services should now be billed using CPT code 96132 for the first hour and 96133 for each additional hour.
Test administration and scoring by a psychologist or neuropsychologist (two or more tests using any method) should now be billed using CPT code 96136 for the first 30 minutes and 96137 for each additional 30 minutes.
Test administration and scoring by a technician (two or more tests using any method) should now be billed using CPT code 96138 for the first 30 minutes and 96139 for each additional 30 minutes.
Single automated test administration should be reported with newly created code 96146 for a single automated psychological or neuropsychological instrument that is administered via electronic platform and formulates an automated result. Psychologists should not use this code if two or more electronic tests are administered and/or if administration is performed by the professional or technician. Instead, the psychologist should use the appropriate codes listed above for test administration and scoring.
Screening and risk assessment (repetitive assessment after screening) include brief emotional/behavioral assessment with scoring and documentation, per standardized instrument, should now be billed using CPT code 96127 separately from testing.
Reference: www.apa.org As we communicated in the October 2019 edition of Provider News, the AIM Rehabilitative program for Anthem’s commercial membership relaunched on November 1. AIM Specialty Health® (AIM), a separate company, is performing prior authorization review of physical (PT), occupational (OT) and speech (ST) therapy services. Prior authorization requests can be submitted via the AIM ProviderPortalSM. The OrthoNet program is no longer active in applicable markets.
The AIM Rehab Program follows the Anthem Clinical Guideline (CG-Rehab-04) that states the skilled services must be delivered by a licensed physical therapist or other qualified licensed health care professional. Qualified providers acting within the scope of their license, including chiropractors, who intend to provide the CPT codes for PT, OT or ST services referenced in this Clinical Guideline should request prior authorization (where permitted by law) for those services through AIM.
In addition, in November we announced the delay of the transition of vendors for review of outpatient PT, OT and ST rehabilitative services for our Medicare members to AIM Specialty Health. The AIM Rehabilitative program for Medicare members will now begin in April 2020; prior authorization will not be required for Medicare members for PT, OT and ST services through March 2020. (Note: This delay does not apply to members for whom prior authorization will still be required.)
Please be sure to check upcoming editions of Provider News for more information about the AIM Rehabilitative Program for Medicare members.
Upcoming changes to AIM’s Rehabilitative Program
Anthem and AIM Specialty Health are working together to make improvements to the clinical review of PT, OT and ST services when used to treat autism spectrum disorder or pervasive developmental delays as defined by the Diagnostic and Statistical Manual of Mental Disorders of the American Psychiatric Association.
We are working to adjust our claims systems to not look for an authorization for commercial members who are receiving skilled treatment for autism spectrum disorder or pervasive developmental delays with one of the following ICD-10 diagnoses: F84.0, F84.2, F84.3, F84.5, F84.8, or F84.9. Until that time, AIM will continue to issue authorizations for PT, OT, and ST services for those diagnoses to help ensure claims are paid appropriately. We will update you once we confirm the effective date of the removal of the prior authorization requirement in our claim system. Please note that while AIM may issue an authorization, benefit limits, if applicable, will still be applied. We value the relationship we have with providers and we always look for opportunities to help expedite claim processing. When a Federal Employee Program® (FEP) member visits your office, please be sure to obtain the most current medical insurance information that will help to establish the primary carrier, alleviate claim denials and support accurate billing. For questions, please contact the Federal Employee Customer Service at 800-722-0203. For more information on copayment/coinsurance requirements and their applicable drug classes, drug lists and changes, prior authorization criteria, procedures for generic substitution, therapeutic interchange, step therapy or other management methods subject to prescribing decisions, and any other requirements, restrictions, or limitations that apply to using certain drugs, visit anthem.com/pharmacyinformation.
The commercial and marketplace drug lists are posted to the website quarterly (the first of the month for January, April, July and October). To locate the Marketplace Select Formulary and pharmacy information, scroll down to ‘Select Drug Lists’, then select the applicable state’s drug list link.
Federal Employee Program (FEP) pharmacy updates and other pharmacy related information may be accessed at www.fepblue.org > Pharmacy Benefits. This drug list is also reviewed and updated regularly as needed. The following clinical criteria documents were endorsed at the September 19, 2019 Clinical Criteria meeting. To access the clinical criteria information please click here.
If you do not have access to the internet, you may request a hard copy of any updated policy by contacting the Provider Call Center.
Revised clinical criteria effective October 14, 2019
(The following clinical criteria was revised to expand medical necessity indications or criteria.)
- ING-CC-0015: Infertility Agents
Revised clinical criteria effective October 14, 2019
(The following clinical criteria were reviewed and may have word changes or clarifications, but had no significant changes to the medical necessity indications or criteria.)
- ING-CC-0007: Synagis (palivizumab)
- ING-CC-0013: Mepsevii (vestronidase alfa)
- ING-CC-0017: Xiaflex (collagenase clostridium histolyticum)
- ING-CC-0018: Lumizyme (alglucosidase alfa)
- ING-CC-0021: Fabrazyme (agalsidase beta)
- ING-CC-0022: Vimizim (elosulfase alfa)
- ING-CC-0023: Naglazyme (galsulfase)
- ING-CC-0024: Elaprase (idursufase)
- ING-CC-0025: Aldurazyme (laronidase)
- ING-CC-0046: Zinplava (bezlotoxumab)
- ING-CC-0058: Octreotide Agents
- ING-CC-0081: Crysvita (burosumab-twza)
Revised clinical criteria effective March 1, 2020
(The following clinical criteria listed below might result in services that were previously covered now being considered not medically necessary.)
- ING-CC-0012: Brineura (cerliponase alfa)
- ING-CC-0072: Selective Vascular Endothelial Growth Factor (VEGF) Antagonists
As a reminder, PCPs may only refer Anthem members to in-network Medicare Advantage providers.
We have contracted with specialists to ensure adequate care of our members. The use of contracted network specialists will ensure continuity of appropriate clinical background data and coordination of care with the PCP.
Should there be a need to refer the member outside the contracted network, contact Anthem directly for prior authorization (PA). Referring a Medicare Advantage member out-of-network, who does not have out-of-network benefits, could result in claim denials with member liability unless the service is urgent, emergent, out-of-area dialysis or if PA was approved by the plan.
Although not required, PA is encouraged for preferred provider organization (PPO) members who want to receive notification of advanced coverage when utilizing an out-of-network provider for services.
As a reminder to all providers, the referring physician name and NPI must be reported on the claim when the PCP does not provide the service rendered. This will help reduce the number of rejections issued during initial claim processing.
The Blue Cross and Blue Shield Association (BCBSA) has issued a mandate with the goal of improving health outcomes and care management for Medicare Advantage members living outside of a control/home plan service area. This mandate will require a change in the way we process the following requests for Medicare Advantage out-of-area (OOA) membership:
- Stars care gap requests
- HEDIS® requests
- Risk adjustment requests
- Medical record requests
This change in process applies to all Blue plans and will go into effect on January 1, 2020.
The current process
The current process for the above-mentioned requests involves the control/home plan sending requests to providers via Inovalon/vendor for medical records and supplemental data to address and/or close an identified or suspected HEDIS® measure, care gap or risk adjustment. Providers receive requests and submit the requested information to the home plan. The home plan receives the information and uses this information, medical records and supplemental data to complete and/or close the request.
The new process
The new process is specific for Medicare Advantage OOA (PPO) members only. These members will be split out from all other members.
For Medicare Advantage OOA members whose home plan is Anthem, the Stars care gap, risk adjustment, HEDIS and medical record requests will be processed via the new BCBSA Provider Engagement Data Exchange (PEX) platform. Anthem as control/home plan will submit these requests to BCBSA via the PEX system. BCBSA will then route the request to the health plan with which the provider is contracted (host plan). The host plan will initiate the provider engagement and gather the requested information (for example, medical records). Providers contracted by the host plan will submit the requested documentation to the plan. The host plan will then submit the documentation via the PEX system to BCBSA. BCBSA will sort the responses and documentation and send to the requesting home plan (member’s home plan).
When Anthem is the host plan, Anthem will receive requests for Stars care gap, risk adjustment, HEDIS and medical record requests from the member’s home plan via the PEX system. Anthem will process the requests, engage providers, and submit requests for medical records and/or supplemental data to the provider. When the provider supplies a response (medical records, supplemental data or additional requests for information), Anthem will send the responses/documentation to the control/home plan via the PEX system. BCBSA will route the responses/documentation to the requesting home plan.
Provider role in new process
Each provider has a key role in the new process. In order to improve the overall care and health outcomes for members, the provider must:
- Respond to requests for medical records and/or supplemental data in a timely manner.
- Request additional information from the provider’s contracted plan, if needed, to complete requests.
- Follow the standard HEDIS, Stars care gap, risk adjustment and medical records requests processes as outlined in the current process.
As a control/home plan, Anthem is taking steps to ensure that providers have the resources needed to complete this new process with little or no impact to the provider’s current operations. Additional provider education resources will be communicated as they become available.
For additional information, please refer to the service numbers on the back of the member’s ID card.
On June 20, 2019, the Pharmacy and Therapeutic (P&T) Committee approved clinical criteria applicable to the medical drug benefit for Anthem. These policies were developed, revised or reviewed to support clinical coding edits.
The clinical criteria are publicly available on the provider website, and the effective dates will be reflected in the link to web posting. Visit Clinical Criteria to search for specific policies.
For questions or additional information, use this email.
Effective January 1, 2020, reimbursement policies will become effective and located on the provider website. AMH Health reimbursement policies apply to providers who serve Medicare Advantage members enrolled in AMH Health. AMH Health reimbursement policies are developed based on nationally accepted industry standards and coding principles. These policies may be superseded by mandates in provider, state, federal or CMS contracts and/or requirements. System logic or setup may prevent the loading of policies into the claims platforms in the same manner as described; however, AMH Health strives to minimize these variations. To view the updated reimbursement policies, visit the provider self‑service website.
What does this mean to providers?
Please refer to the reimbursement policy website, your provider manual and/or your provider contract as a guide for reimbursement criteria. Reimbursement policies serve as a guide to assist you in accurate claim submissions and to outline the basis for reimbursement if the service is covered by a member’s benefit plan. The determination that a service, procedure, item, etc. is covered under a member's benefit plan is not a determination that you will be reimbursed. Services must meet authorization and medical necessity guidelines appropriate to the procedure and diagnosis, as well as to the member’s state of residence. Proper billing and submission guidelines are required along with the use of industry-standard, compliant codes on all claim submissions.
We reserve the right to review and revise our policies when necessary. Reimbursement policies go through a review every two years for updates to state, federal or CMS contracts and/or requirements. When there is an update, we will publish the most current policy at the provider website.
Code and clinical editing
AMH Health applies code and clinical editing guidelines to evaluate claims for accuracy and adherence to accepted national industry standards and plan benefits. We use sophisticated software products to ensure compliance with standard code edits and rules. These products increase consistency of payment for providers by ensuring correct coding and billing practices. Editing sources include but are not limited to CMS National Correct Coding Initiative, Medical Policies and Clinical Utilization Management Guidelines. AMH Health is committed to working with you to ensure timely processing and payment of claims.
For assistance
The complete set of policies is available at the provider website. If you have questions, please visit the provider self-service website or call the number on the back of the member’s ID card.
Use this tool to initiate Anthem | MaineHealth inpatient and outpatient medical prior authorization requests online
As we communicated in this issue of Provider News, MaineHealth and Anthem will offer Medicare Advantage plans in 2020 under the Anthem | MaineHealth brand. We’re pleased to announce that beginning January 1, 2020, your practice can initiate online prior authorization (PA) requests for Anthem | MaineHealth members efficiently and conveniently with our Interactive Care Reviewer (ICR) tool available through the Availity Portal. The ICR offers a streamlined process to request inpatient and outpatient procedures. ICR is available for Anthem | MaineHealth and Anthem Medicare Advantage at this time. It is not yet available for Anthem commercial authorizations.
How do I gain access to the ICR?
You can access our ICR tool via the Availity Portal. If your organization has not yet registered for Availity, go to www.availity.com and select Register in the upper right-hand corner of the page.
If your organization already has access to Availity, your Availity administrator can grant you access to the Authorization and Referral Request for submission capability, and Authorization and Referral Inquiry for inquiry capability. You can then find our tool under Patient Registration > Authorizations & Referrals. From this area, you can select the Authorizations or Authorization/Referral Inquiry option as appropriate.
Whom can I contact with questions?
For questions on accessing our tool via Availity, call Availity Client Services at 1-800-AVAILITY. Availity Client Services is available Monday through Friday from 8:00 a.m. to 7:00 p.m. (excluding holidays) to answer your registration questions.
Register and attend one of the ICR monthly webinars.
What benefits/efficiencies does the ICR provide for Anthem | Maine Health and Anthem Medicare Advantage authorizations?
ICR:
- Can determine if PA is needed. For most requests, when you enter patient, service and provider details, you will receive a message indicating whether review is required.
- Provides inquiry capability. Ordering and servicing physicians and facilities can locate information on PA requests for those they are affiliated with; this includes requests previously submitted via phone, fax and ICR.
- Reduces the need to fax. The ICR allows text detail and images to be submitted along with the request. Therefore, you can submit requests online and reduce the need to fax medical records.
- Is available with no additional cost to you. The ICR is a no-cost solution that’s easy to learn and even easier to use.
- Is accessible from almost anywhere. You can submit your requests from any computer with internet access. (Note: We recommend you use Internet Explorer 11, Chrome, Firefox or Safari for optimal viewing.)
- Provides a comprehensive view of all of your PA requests. You have a complete view of all the utilization management requests you submitted online, including the status of your requests and specific views that provide case updates and a copy of associated letters.
|