Provider News GeorgiaJuly 1, 2022 July 2022 Anthem Provider News - GeorgiaPlease note that the important message below from Bryony Winn – President, Health Solutions – applies to our Commercial, Medicaid and Medicare Advantage programs from Anthem Blue Cross and Blue Shield.
I am pleased to announce that our shareholders voted to approve our parent company's name change from Anthem, Inc. to Elevance Health, Inc. (NYSE Ticker Symbol — ELV) effective
June 28, 2022.
Here is what you can expect:
- A bold new vision for the future of health
We chose the name Elevance Health to better reflect our business as we elevate the importance of whole health and advance health beyond healthcare for consumers, their families, and our shared communities. This new vision fuels our transformation from a traditional health benefits organization to a health company that looks beyond the traditional scope of physical health.
- No action is needed by you, and we remain committed to helping you deliver whole-person care for your patients, our customers. Importantly, there is no impact or changes to your contract, reimbursement, or level of support. For your patients, it will not change their plan or coverage or change how they receive their medications. Provider networks will not be changing.
- A more holistic approach to health that improves affordability and outcomes
Bringing together a broad portfolio of health plans, including pharmacy, behavioral, clinical, and complex care provider partners, we can deliver integrated, holistic health solutions to meet the increasing needs of our customers and care provider partners. This includes two notable changes:
- Our healthcare service partners will operate under a new brand called Carelon. This includes Beacon Health Options, AIM Specialty Health®, CareMore, and IngenioRx. You can find us at Carelon.com.
- IngenioRx, our pharmacy benefit management partner, will become CarelonRx on
January 1, 2023. This name change will not impact your patient’s benefits, coverage, or how their medications are filled. We will communicate detailed information about this change soon.
- A simpler brand portfolio that makes it easier to do business with us
We have streamlined and simplified the complexity of our health plan and service businesses and reduced the number of brands we have in the market, so our partners and customers clearly understand where we serve, who we serve, and what our brands do.
What does this mean for care providers?
We will operate as Anthem Blue Cross or Anthem Blue Cross and Blue Shield in our 14 Blue-licensed markets. Our existing Anthem-branded health plans are not changing and will continue to operate in their current states. There will be no impact to plans, coverage, or level of support.
Looking forward together
As your partner, we will continue to keep you updated with new information as soon as it becomes available. In the meantime, you can visit us at ElevanceHealth.com or contact your provider representative with any questions.
Thank you for joining us on this exciting path forward as we reimagine what is possible for every moment of health.
Sincerely,

Bryony Winn
President, Health Solutions
ATTACHMENTS (available on web): Bryony Sig.jpg (jpg - 0.01mb) Current provider directory information helps Anthem Blue Cross and Blue Shield members find the most up-to-date information available. As a partner in the care of our members, we ask that you review your online provider directory information regularly and provide updates as needed.
If changes are needed, please take the time to update your information by submitting updates and corrections to us on our online Provider Maintenance Form. Online update options include:
- Adding/changing an address location
- Name change
- Tax ID changes
- Provider leaving a group or a single location
- Phone/fax number changes
- Closing a practice location
Once you submit the Provider Maintenance Form, you will receive an email acknowledging receipt of your request. Visit the Provider Maintenance Form landing page for complete instructions.
The Consolidated Appropriations Act (CAA), effective January 1, 2022, contains a provision that requires online provider directory information be reviewed and updated (if needed) at least every 90 days. Thank you for doing your part in keeping our provider directories current.
Effective for all claims received on or after August 1, 2022, in accordance with the Anthem Blue Cross and Blue Shield (Anthem) reimbursement policy titled Implant — Facility, we will implement additional steps to review claims submitted by facilities that inappropriately include supply HCPCS codes (HCPCS codes for catheters, needles, guidewires) billed with implant revenue codes (for example, 0278).
Anthem considers implants to be medical devices that remain in the member’s body upon discharge from the procedure. Therefore, supplies are not considered implants. Claims for supplies should be submitted with the appropriate revenue code(s). Claim lines billed inappropriately will be denied. Providers can resubmit claim for supplies using the appropriate revenue code(s).
If you have questions about this policy, contact your contract manager or Provider Experience representative.
We are enhancing our outpatient facility editing to help align with correct coding guidelines for usage of HCPCS code G0463. The code description for G0463 is “hospital outpatient clinic visit or assessment and management of a patient”. Based on this code description, HCPCS code G0463, should only be billed with revenue codes which support the billing of clinic visits/assessment & management services. When G0463 is billed with an inappropriate revenue code, it will be denied. For assistance with coding guidelines, the National Uniform Billing Committee (NUBC) is a valuable resource.
3072F: new language about two-year compliance.
The Comprehensive Diabetes Care HEDIS® measure Retinal Eye Exam (DRE) valuates the percent of adult members ages 18 to 75, with diabetes (type 1 and type 2), who had a retinal eye exam during the measurement year.
Changes to 3072F
The definition for the code 3072F (negative for retinopathy) has been redefined to low risk for retinopathy (no evidence of retinopathy in the prior year). This can be particularly confusing because it would not be used at the time of the exam. It would be used the following year, along with the exam coding for the current year, to indicate that retinopathy was not present the previous year.
A simpler coding solution
Using these three codes count toward the DRE measurement if they are billed in the current measurement year or the prior year. This means you can submit the appropriate code at the time of the exam, and it covers both years:
|
2023F
|
Dilated retinal eye exam with interpretation by an ophthalmologist or optometrist documented and reviewed; without evidence of retinopathy (DM)
|
|
2025F
|
7 standard field stereoscopic retinal photos with interpretation by an ophthalmologist or optometrist documented and reviewed: without evidence of retinopathy (DM)
|
|
2033F
|
Eye imaging validated to match diagnosis from 7 standard field stereoscopic retinal photos results documented and reviewed: without evidence of retinopathy (DM)
|
For more about diabetic retinopathy, visit CMS.gov or use this link to read more.
Meeting the measurement for all diabetes care
These exams are also important in evaluating the overall health of diabetic patients, as well as meeting the Comprehensive Diabetes Care HEDIS measure:
- Hemoglobin A1c (HbA1c) testing
- HbA1c poor control (> 9.0%)
- HbA1c control (< 8.0%)
- Retinal Eye exam performed
- Blood Pressure control (< 140/90 mm Hg)
Record your efforts in the member’s medical records for the HbA1c tests and results, retinal eye exam, blood pressure, urine creatinine test, and the estimated glomerular filtration rate test. Meeting the mark and closing gaps in care is key to good health outcomes.
In a recent study published by Pediatrics, economic hardship, school closing, and shutdowns led to sedentary lifestyles and increases in childhood obesity. The research analyzed doctor visits pre-pandemic then during the pandemic period, and the increases were dramatic. Overall obesity increased from 13.7% to 15.4% in patients 5 to 9 years. Increases from 1% in children aged 13 to 17 to 2.6% for those aged 5 to 9 years were observed.
The study recommended new approaches to Weight Assessment and Counseling. These include recommending virtual activities that promote increased physical activity. Focusing on ways to remain safe and active with outside activities, such as park visits, walks, and bike riding were also suggested.
The Centers for Disease Control and Prevention has a great resource called Ways to Promote Health with Preschoolers. This fun flyer shows how we can all work together to support a healthy lifestyle. You can download a copy here.
The HEDIS® measure Weight Assessment and Counseling for Nutrition and Physical Activity for Children/Adolescents (WCC) requires a nutritional evaluation and pro-active guidance as part of a routine health visit:
- When counseling for nutrition, document current nutritional behavior, such as meal patterns, eating and diet habits, and weight counseling.
- When counseling for physical activity, document current physical activity behavior, such as exercise routine, participation in sports activities, bike riding and play groups.
- Handouts about nutrition and physical activity also count toward meeting this HEDIS measure when documented in the member’s health record.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA).
HEDIS® measure WCC looks at the percentage of members, 3 to 17 years of age, who had an outpatient visit with a PCP or OB/GYN and have documented evidence for all the following during the measurement year:
- Body mass index (BMI) percentile (percentage, not value).
- Counseling for nutrition.
- Counseling for physical activity.
Telehealth, virtual check-in, and telephone visits all meet the criteria for nutrition and physical activity counseling. Counseling does not need to take place only during a well-visit, WCC can also be completed during sick visits. Documenting guidance in your patient’s records is key.
Code services correctly to measure success.
These diagnosis and procedure codes are used to document BMI percentile, weight assessment, and counseling for nutrition and physical activity:
|
Description
|
CPT®
|
ICD-10-CM
|
HCPCS
|
|
BMI percentile
|
|
Z68.51-Z68.54
|
|
|
Counseling for nutrition
|
97802, 97803,
97804
|
Z71.3
|
G0270, G0271, G0447, S9449,
S9452, S9470
|
|
Counseling for physical activity
|
|
Z02.5, Z71.82
|
G0447, S9451
|
|
Codes to identify outpatient visits:
CPT — 99201-99205, 99211-99215, 99241-99245, 99341-99345, 99347-99350, 99381-99387, 99391-99397, 99401-99404, 99411, 99412, 99429, 99455, 99456, 99483
HCPCS — G0402, G0438, G0439, G0463, T1015
|
|
American Academy of Pediatrics. American Academy of Pediatrics raises concern about children’s nutrition and physical activity during pandemic. Available at: http://services.aap.org/en/news-room/news-releases/aap/2020/american-academy-of-pediatrics-raises-concern-about-childrens-nutrition-and-physical-activity-during-pandemic/. Accessed December 10, 2020.
The Provider Manual has been updated for an effective date of October 1, 2022, and is now available on our website. To view the updated manual, go to anthem.com. Select Providers and then under Provider Resources, select Policies, Guidelines and Manuals. Enter Georgia as state, scroll to Provider Manual and select Download the Manual.
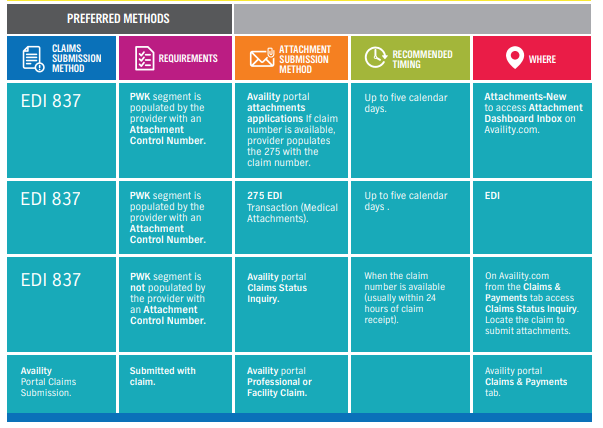
Submitting attachments electronically is the most efficient way for you to receive your claim payments faster — that’s why we have been hard at work making the digital attachment process easier, more intuitive, and streamlined.
We’re preparing to launch an enhancement to the Claims Status Inquiry application that will enable you to submit claims attachments directly to the claim from Availity.com.
Submitting attachments electronically:
- Reduces costs associated with manual submission.
- Reduces errors associated with matching the claim when attachments are submitted manually.
- Reduces delays in payments.
- Saves time: No need to copy, fax, or mail.
- Reduces the exchange of unnecessary member information and too much personal health information sharing.
If your workflow for attachments is through EDI submissions or directly through the Availity application, we have a solution for that.
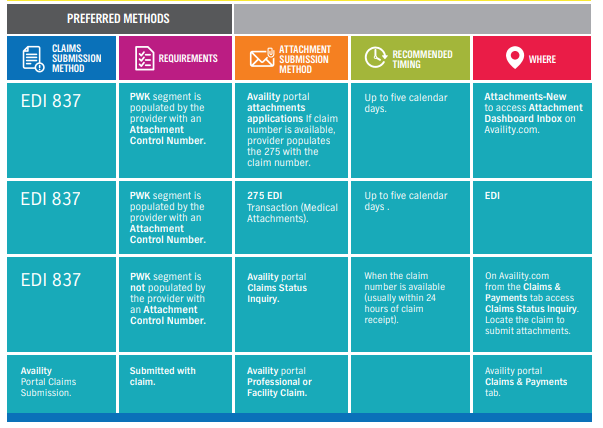
Didn’t submit your attachment with your claim? No problem!
If you submitted your claim through EDI using the 837, and the PWK segment contains the attachment control number, there are three options for submitting attachments:
- Through the attachments dashboard inbox:
- From com, select the Claims & Payments tab to access Attachments – New and your Attachments Dashboard Inbox
- Through the 275 attachment:
- Important: You must populate the PWK segment on the 837 with your document control number to ensure the claim can match to the attachment.
- Through the Availity.com application:
- From com, select the Claims & Payments tab to run a Claims Status Inquiry to locate your claim. When you have found your claim, select the Send Attachments button:
- If you submitted your claim through the Availity application, simply submit your attachment with your claim
- If you need to add additional attachments, to add a forgotten attachment, or for claims adjustments:
- From com, select the Claims & Payments tab and run a Claims Status Inquiry to locate your claim. When you have found your claim, use the Send Attachments button.
For more information and educational webinars
In collaboration with Availity, we will hold a series of educational webinars that includes a deep dive into EDI attachment submissions, as well as the new Claims Status Inquiry workflow. Sign up today.
ATTACHMENTS (available on web): 2397 Image.png (png - 0.09mb) Anthem Blue Cross and Blue Shield is setting up a new digital education platform called the Provider Learning Hub. Initially, the Provider Learning Hub will include how-to instructions for Availity* registration and onboarding. Our first featured training is focused on the Attachment application with special emphasis on new processes that should make submitting attachments more efficient.
You can access the new Provider Learning Hub from the home page on our public website under Important Announcements in mid-July or by navigating to this link: https://gateway.on24.com/wcc/eh/3555851/category/104185/anthem-blue-cross-and-blue-shield.
This communication applies to the Commercial and Medicare Advantage programs from
Anthem Blue Cross and Blue Shield (Anthem).
In an effort to deliver on Anthem’s purpose to improve the health of humanity, we now have a program for in-home patient care for acute conditions.
Anthem’s Hospital in Home program can advise capable, innovative hospital partners in developing their own hospital in home programs. Once implemented, patients can recover in a more comfortable environment, allowing hospitals to keep beds available for patients with more complex needs.
Inpatient level of care in the home can be a welcome alternative to traditional hospital settings. Patients may find acute care at home to be more convenient and less stressful, and studies have shown acute care at home can be safe and allow for smoother transition to self-care management after the acute illness. Hospital in Home clinical trials demonstrate a 25% decrease in readmissions and a 50% reduction in time spent in bed.1
Anthem’s Hospital in Home program has a set of minimum requirements that are designed to promote patient safety. These requirements include aspects of the member’s home environment, the clinical scenario, remote monitoring capabilities, and plans for program evaluation.
Please contact your Anthem contracting representative to learn more about Anthem’s Hospital in Home program.
Effective December 31, 2022, the enhanced reimbursement billing opportunity (S-codes) for medical oncologists selecting on-pathway drug regimens as part of the AIM Specialty Health ®* Medical Oncology Solution/ Cancer Care Quality Program (CCQP) chemotherapy authorization process will be discontinued.
The CCQP S-codes S0353 and S0354 were activated on July 1, 2014, and have supported providers with member care coordination, and adoption of optimal, evidence-based oncology drug regimens.
The CCQP/AIM pathways will continue to enable the delivery of clinically appropriate cancer treatment, and supportive medication that ensures members receive high-quality, patient-centered care. The AIM pathways will remain available to medical oncologists and related subspeciality providers via the AIM provider website.
As the CCQP continues to evolve, the program will become a key component of more comprehensive value-based cancer care improvement initiatives, including the Oncology Medical Home Plus (OMH+) program, launching on July 1, 2022, and January 1, 2023.
Contact your Anthem Blue Cross and Blue Shield network representative or your oncology provider engagement liaison for more information.
Material adverse change
Beginning with dates of service on or after October 1, 2022, Anthem Blue Cross and Blue Shield (Anthem) will update the Modifiers Impacting Adjudication code list to not allow reimbursement for CPT® code 99211 when appended with a modifier 25.
For specific policy details, visit the reimbursement policy page at anthem.com provider website.
Material adverse change
Beginning with dates of service on or after October 1, 2022, the Anthem Blue Cross and Blue Shield Laboratory and Venipuncture Services policy is expanded to include facility providers. The related coding section is updated to clarify coding for professional and facility providers.
Facility providers are not eligible for separate reimbursement for the following select
specimen-handling CPT®/HCPCS codes: 99000, 99001, H0048, P9603, and P9604. In addition, Related Coding section 1 in the Bundled Services and Supplies policy is updated to remove these codes.
For specific policy details, visit the reimbursement policy page at anthem.com provider website.
Material adverse change
Beginning with dates of service on or after October 1, 2022, Anthem Blue Cross and Blue Shield (Anthem) will implement a new professional and facility reimbursement policy titled, Modifier FB — Professional and Facility. Modifier FB should be appended to all devices, supplies, or drugs obtained at no cost to the provider. Services appended with modifier FB are not eligible for reimbursement.
In addition, Modifier FB has been removed from the Modifier Rules — Professional policy.
For specific policy details, visit the reimbursement policy page at anthem.com provider website.
In the September 2021 edition of Provider News, we announced that a new commercial reimbursement policy titled ‘Sexually Transmitted Infections - professional’ would be effective for dates of service on or after December 1, 2021. We have made a decision to retract this reimbursement policy.
Material adverse change
Beginning with dates of service on or after October 1, 2022, Anthem Blue Cross and Blue Shield will implement the following:
- 96365, 96369, 96372, 96373, 96374, 96379 will deny when reported with 78265, 78830 or 78835.
- 95957 will deny when reported with 95700 on the same day:
- The reference to subsequent dates of service was removed from this code pair.
For specific policy details, visit the Reimbursement Policy page on the provider website.
Anthem Blue Cross and Blue Shield (Anthem) has added value to the Transitional Care Management definition to include discharge from the emergency room to help prevent future emergency room encounters or hospital admissions.
As of April 27, 2022, Anthem has implemented a new professional reimbursement policy: Transitional Care Management. When a member requires a transition to a community setting, the Transitional Care Management period begins upon the member’s discharge and continues for 29 days.
For specific policy details, visit the Reimbursement Policy page on the provider website.
Material adverse change
Beginning with dates of service on or after October 1, 2022, Anthem Blue Cross and Blue Shield will update the policy language to indicate the following:
- The title of the policy will be renamed to Place of Service – Facility from Place of Service Evaluation and Management Services – Facility.
- Professional services billed under revenue codes 960-983 are nonreimbursable when submitted on a UB-04.
- Preventive Counseling CPTs 99406–99409, 99411, and 99412 are nonreimburseable when billed in an outpatient setting.
As a reminder, Evaluation and Management (E/M) services and other professional services (excluding evaluation and management services rendered in the emergency room and billed with ER revenue codes) are required to be billed on a CMS 1500 form.
For specific policy details, visit the reimbursement policy page at anthem.com provider website.
The Blue Cross and Blue Shield Service Benefit Plan, aka Federal Employee Program® (FEP) is now providing a Concierge Cancer Care program as part of the benefit package. Members in Georgia, newly diagnosed with cancer will be provided an opportunity to have at no charge a second opinion by a board-certified oncologist from The Clinic-Cleveland Clinic.

The FEP Concierge Cancer Care program helps members along each step of their cancer journey by providing support and resources to navigate the healthcare system. The program’s team of compassionate and caring professionals will review member treatment options, answer their questions, check in along the way, and take as much of the burden off them and their primary medical oncology team as possible, allowing members to focus on their health and recovery. Concierge Cancer Care program includes:
- Virtual second opinion: The program makes it easy for newly diagnosed cancer patients’ records to be shared with additional oncologists for review.
- Access to clinical trials: The program matches members with clinical trials when appropriate and ensures they have timely access to the selected program, alleviating the financial barriers to participating, such as transportation and lodging for a member and guest; the only member costs are standard medical plan copays and deductibles.
- Partnership with Centers of Excellence across the U.S.
- Remote monitoring technology: Tytocare handheld exam kits allow Anthem Blue Cross and Blue Shield (Anthem) LiveHealth Online healthcare providers to provide round-the-clock support triaging symptoms and side effects — accessing members’ vital signs and performing remote physical exams, potentially decreasing the need for stressful visits emergency or urgent care visits and avoiding exposure while members are immuno-compromised.
- End-to-end support: Program staff stay connected with members during every step, ensuring they know what to expect.
Georgia FEP members will receive a call or email from The Clinic-Cleveland Clinic to allow the member to opt in or opt out of a virtual second opinion.
Learn more about how the Blue Cross and Blue Shield Service Benefit Plan, aka Federal Employee Program (FEP) is communicating this benefit to members in Georgia.
ATTACHMENTS (available on web): 2030.jpg (jpg - 0.02mb) Visit the Drug Lists page for more information on:
- Copayment/coinsurance requirements and their applicable drug classes.
- Drug lists and changes.
- Prior authorization criteria.
- Procedures for generic substitution.
- Therapeutic interchange.
- Step therapy or other management methods subject to prescribing decisions.
- Any other requirements, restrictions, or limitations that apply to using certain drugs.
The commercial and marketplace drug lists are posted to the website quarterly on the first day of the month in January, April, July, and October.
To locate Marketplace Select Formulary and pharmacy information, scroll down to Select Drug Lists. This drug list is also reviewed and updated regularly as needed.
Federal Employee Program Pharmacy updates and other pharmacy related information may be accessed at www.fepblue.org > Pharmacy Benefits.
Effective for dates of service on and after October 1, 2022, the following current clinical criteria were revised and might result in services that were previously covered but may now be found to be not medically necessary:
|
Document number
|
Clinical criteria
|
|
ING-CC-0200
|
Aduhelm (aducanumab)
|
Access the clinical criteria document information.
Anthem Blue Cross and Blue Shield (Anthem)’s prior authorization clinical review of non-oncology specialty pharmacy drugs will be managed by Anthem’s medical specialty drug review team. Oncology drugs will be managed by AIM Specialty Health® (AIM), a separate company.
Medicare Advantage
Beginning with claims processed on or after August 1, 2022, Anthem Blue Cross and Blue Shield will implement additional steps to review claims for evaluation and management (E/M) services submitted by professional providers when a preventive service (CPT® codes 99381 to 99397) is billed with a problem-oriented E/M service (CPT codes 99202 to 99215) and appended with Modifier 25 (for example, CPT code 99393 billed with CPT code 99213 to 99225).
According to the American Medical Association (AMA) CPT Guidelines, E/M services must be “significant and separately identifiable” in order to appropriately append Modifier 25. Based upon review of the submitted claim information, if the problem-oriented E/M service is determined not to be a significant, separately identifiable service from the preventive service, the problem-oriented E/M service will be bundled with the preventive service.
Providers that believe their medical record documentation supports a significant and separately identifiable E/M service should follow the Claims Payment Dispute process (including submission of such with the dispute) as outlined in the provider manual.
If you have questions on this program, contact your contract manager or Provider Experience.
Medicare Advantage
This communication applies to the Commercial and Medicare Advantage programs from
Anthem Blue Cross and Blue Shield (Anthem).
In an effort to deliver on Anthem’s purpose to improve the health of humanity, we now have a program for in-home patient care for acute conditions.
Anthem’s Hospital in Home program can advise capable, innovative hospital partners in developing their own hospital in home programs. Once implemented, patients can recover in a more comfortable environment, allowing hospitals to keep beds available for patients with more complex needs.
Inpatient level of care in the home can be a welcome alternative to traditional hospital settings. Patients may find acute care at home to be more convenient and less stressful, and studies have shown acute care at home can be safe and allow for smoother transition to self-care management after the acute illness. Hospital in Home clinical trials demonstrate a 25% decrease in readmissions and a 50% reduction in time spent in bed.1
Anthem’s Hospital in Home program has a set of minimum requirements that are designed to promote patient safety. These requirements include aspects of the member’s home environment, the clinical scenario, remote monitoring capabilities, and plans for program evaluation.
Please contact your Anthem contracting representative to learn more about Anthem’s Hospital in Home program.
Medicare Advantage
The Cancer Care Navigator (CCN) program is a comprehensive cancer support solution for oncologists and Anthem Blue Cross and Blue Shield (Anthem) members who are at high risk for complications during treatment. This program is aimed at helping to simplify the complexities of cancer care for members.
Practices are given a single point of contact to connect the practice to the right people at Anthem to help lessen administrative burdens. CCN also gives the practice access to Anthem’s advanced predictive analytics to help identify patients at high risk for complications, in turn allowing providers the opportunity to take preventive action and guide targeted interventions.
Patients are provided with a wealth of support through supplemental services (dietitians, pharmacists, etc.), medication adherence assistance, individualized care plans, and goal setting, as well as after-hours telephonic and digital support.
CCN is the ultimate support service to improve the care experience and quality of life to allow patients time to focus on overall health and well-being. Please feel free to reach out to the CCN team at 866-649-0669.
|