Provider News ColoradoNovember 1, 2023 November 2023 Provider Newsletter Featured Articles Digital Solutions | Commercial | October 31, 2023 Digital Solutions | Commercial / Medicare Advantage | October 31, 2023 Education & Training | Commercial | October 31, 2023
COBCBS-CRCM-041559-23 HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). Effective for claims processed on or after December 1, 2023, the editing systems at Anthem Blue Cross and Blue Shield will be updated to align with the American Medical Association (AMA) CPT® Manual, HPCPS Level II Manual, and Centers for Medicare & Medicaid Services (CMS) correct coding guidelines, for the following services: Ulcer debridement and ulcer staging:- According to the ICD-10 Diagnosis Coding Manual, specific diagnosis codes that reflect the stage of the ulcer should be billed with the appropriate CPT code. For example, if billing a stage 3 pressure ulcer code, a stage 4 diagnosis code should not be reported.
- According to the AMA CPT Manual, a debridement of an ulcer should be reported with the appropriate diagnosis code that reflects that service.
Billing of anatomical modifiers:- According to the AMA CPT and HCPCS Level II manuals, the appropriate anatomical modifier is required to be appended to the appropriate procedure code. If not, the claim line will be denied. These modifiers designate the body part that a service is being performed on (for example, FA: Left hand, thumb, TA: Left foot, great toe).
Billing of interprofessional telephone/internet consultations:- These billed procedure codes will follow the AMA CPT Manual coding guidelines.
Claim lines not billed in accordance with the correct coding guidance outlined above will be denied. If you disagree with a claim reimbursement decision, please follow the claim dispute process (including submission of such documentation with the dispute) as outlined in the Provider Manual. If you have questions about this communication or need assistance with any other item, contact your provider relationship management representative. With your help, we can continually build towards a future of shared success. Anthem Blue Cross and Blue Shield is the trade name of Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc. Independent licensees of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-038660-23, MULTI-BCBS-CR-046278-23-CPN45683 The Centers for Medicare and Medicaid Services (CMS) has provided specific guidance regarding the usage of the following modifiers: Modifier | Description | GA | Waiver of Liability statement issued as required by payer policy. | GX | Notice of Liability issued, voluntary under payer policy. | GY | Item or Service Statutorily Excluded, does not meet the definition of any Medicare benefit. | GZ | Item or service expected to be denied as not reasonable and necessary. |
It has been determined that these modifiers were used inappropriately for Medicare Advantage (MA) members. Examples include: - The member has an enhanced or supplemental benefit above what original Medicare covers and one or more of the above modifiers are applied to the claim:
- Such as office calls billed by a chiropractor and the service is an enhanced benefit under the member’s Medicare Advantage health plan.
- The item/service is a covered benefit but one or more of the above modifiers is applied to claim:
- Such as 911 ambulance calls:
- CMS guidance states that if the call is in accordance with a prudent layperson’s definition of emergency medical condition, regardless of the final diagnosis.
An Advance Beneficiary Notice (ABN) is a written notice given to an original Medicare beneficiary by a provider (including physicians, practitioners, durable medical equipment (DME) companies, laboratories, etc.) when they believe that Original Medicare will deny some or all of the services or items because of medical necessity or the frequency of the service; however, the ABN is optional when original Medicare never covers a service or item. When a provider obtains an ABN along with the original Medicare requirements, the provider may indicate that they have obtained an ABN by billed with modifier GS, GX, GY and/or GZ. As published in the Medicare Claims Processing Manual, Chapter 30, Section 50, the ABN is provided to original Medicare beneficiaries for the above scenarios and is not used for items or services provided/denied under the MA program or for prescription drugs provided under the Medicare Prescription Drug Program (Part D). Under the MA program, MA members and their providers have the option to obtain a coverage decision prior to obtaining the item or service. This request for a pre-service coverage review is known as a request for an organizational determination. Because a MA member can obtain a pre-service coverage decision through the pre-service organizational determination process, the use of the ABN for MA members is not appropriate. This means that the liability modifiers that denote that there is an ABN on file is not appropriate for MA members. Providers (contracted and non-contracted providers as well as members) have the ability to request an organizational determination (prior authorization) prior to providing an item or service to determine if the item or service will be covered under the member’s health plan benefits. Once an organizational determination has been made, if a denial is warranted, an Integrated Denial Notice (IDN) will be sent to the member and provider. This document provides important appeal rights guaranteed to the member. If the service is denied, the member will be better informed to choose if they would still like to obtain the item or service at their own expense. Claims are not processed based on the G modifier, but rather on the benefit of the service rendered. MULTI-BCBS-CR-040516-23-CPN39023 The Consolidated Appropriations Act (CAA) of 2021 contains a provision that requires online provider directory information be reviewed and updated as needed at least every 90 days. Maintaining your online provider directory information is essential for members and healthcare partners to connect with you when needed. Please review your information frequently and let us know if any of your information we show in our online directory has changed. Submit updates and corrections to your directory information by following the instructions on our Provider Maintenance webpage. Online update options include: - Add/change an address location.
- Name change.
- Provider leaving a group or a single location.
- Phone/fax number changes.
- Closing a practice location.
Reviewing your information helps us ensure your online provider directory information is current. Through genuine collaboration, we can simplify access to care and help you deliver high-quality, equitable healthcare. MULTI-BCBS-CM-040987-23-SRS40837 Digital RFAI providers: The progress dashboard is now available! Transparency at your fingertipsProviders enrolled in the Medical Attachments applications on Availity are taking advantage of faster claims processing through Digital Request for Additional Information (Digital RFAI). They are receiving digital notifications when additional documents are needed to process our members’ claims. 
We receive the documentation faster, so the claim is processed faster, too.If seeing is believing, Digital RFAI providers will want to use the Digital RFAI Progress Dashboard right away. Track the number of document submissions, processing turnaround time, payment turnaround time, types of documents requested, and more. Use filters to customize the report and reporting period. Access the Digital RFAI Progress Dashboard from Availity.com through Payer Spaces. Use this link for the Quick Reference Guide. Providers need an Availity registration to access the Quick Reference Guide. Not a Digital RFAI provider?If you’re not already using the Digital RFAI process and want to take advantage of faster claims processing, participation is easy! Learn more!Use this link to register for live training or to view the live training on-demand. Digital RFAI process improvements: Eliminating the acknowledgement boxSaving steps and streamlining processes We have eliminated the acknowledgement requirement when providers access their Attachments Dashboard. You’ll notice that notifications on your Attachments Dashboard have a New status. Saving you time: When you click on the claim, you are no longer required to complete the acknowledgement. You will be diverted directly to the notification information. Added transparency: If you upload your notification and select Save, we have created a Saved status that dates your upload. Your feedback is important to us and helps us to enhance the process and create greater efficiencies for you and your practice. Reach out to your provider relationship management representative with additional feedback or if you have additional questions. MULTI-BCBS-CM-041232-23-CPN41101 As we communicated in October, Availity Essentials Provider Data Management (PDM) is now available as the intake application for care providers to submit demographic change requests, including submitting roster uploads. As of January 1, 2024, Availity Essentials PDM will replace all current intake channels for demographic change requests and roster submissions. Providers should continue to utilize the Provider Enrollment application in Availity Essentials to submit requests to add new practitioners under existing groups. Read the previously published articles here: Take action nowDon’t wait until January to start using the Availity Essentials PDM application. Start using it today to take advantage of the benefits of these options and familiarize yourself with the process before the legacy intake channels retire. Benefits to our care providers using Availity Essentials PDMThe Availity Essentials PDM application will ensure the following: - Attest and manage current provider demographic information
- Consistently updated data
- Decreased turnaround time for updates
- Compliance with federal and/or state mandates
- Improved data quality through standardization
- Increased provider directory accuracy
Choice and flexibility to select the option that works best for youRequest data updates via either one of the following options within Availity Essentials PDM: - Multi-payer platform option: allows providers to make updates once and have that information sent to all participating health plans, submitting each change separately
- Roster upload option: allows providers to submit multiple updates within one spreadsheet via the Upload Rosters feature:
- The Upload Roster feature is currently only available, and shared with, Anthem.
Want to submit a roster using Availity Essentials PDM?Now you can. Roster Automation is our new technology solution designed to streamline and automate provider data additions, changes, and terminations that are submitted using a standardized Microsoft Excel submission. Any provider, whether an individual provider/practitioner, group, or facility, can use Roster Automation today:* - Utilize the Roster Automation Standard Template:
- Follow the Roster Automation Rules of Engagement: Find it online at https://tinyurl.com/mw57cc49:
- This reference document is available to ensure error-free submissions, driving accurate and more timely updates through automation.
- More detailed instructions on formatting and submission requirements can also be found on the first tab of the Roster Automation Standard Template (User Reference Guide).
- Upload your completed roster via the Availity Essentials PDM application.
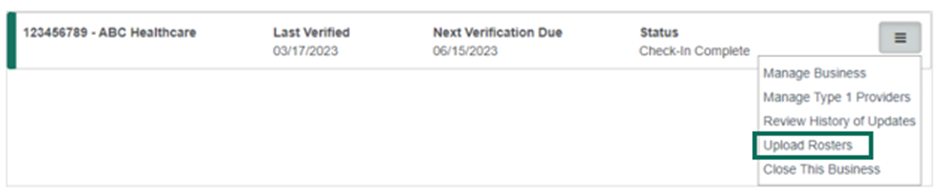
What about the previous methods by which i have been submitting information?While we are in the process of sunsetting our legacy intake channels, we will continue to process submissions received through current intake channels until December 31, 2023. Effective January 1, 2024, all PDM requests, including rosters, must be submitted via Availity Essentials PDM. As of this date, all provider demographic change requests, including rosters, will be rejected if submitted through any format/channel other than Availity Essentials PDM. Again, if preferred, providers may continue to utilize the Provider Enrollment application in Availity Essentials to submit requests to add new practitioners under existing groups. How to access the Availity Essentials PDM applicationLog onto Availity.com and select My Providers > Provider Data Management to begin the attestation process. If submitting a roster, find the TIN/business name for which you want to verify and update information. Before you select the TIN/business name, select the three-bar menu option on the right side of the window, and select Upload Rosters (see screen shot below) and follow the prompts. 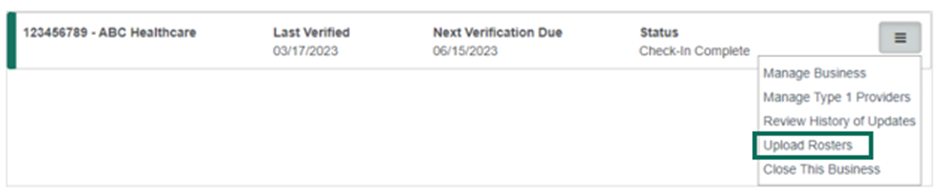 Availity administrators will automatically be granted access to PDM. Additional staff may be given access to Provider Data Management by your Availity administrator. To find your Availity administrator, go to My Account Dashboard > My Account > Organization(s) > Administrator Information. Training is available:- Availity Essentials PDM application specific training:
- An Availity account is required for accessing these training options. If not registered yet, see end of this article for registration details:
- Learn about and attend one of our live webinars by visiting here. Note: You must log into Availity first. Then, select the link.
- View the Availity Essentials PDM quick start guide online by visiting here. Note: You must log into Availity first. Then, select the link.
- Roster Automation Template and Rules of Engagement specific training:
- Thursday, November 16, 4-5pm ET — Register November 16, 2023.
- Wednesday, November 29, 4-5pm ET — Register November 29, 2023.
- Wednesday, December 6, 4-5pm ET — Register December 6, 2023.
- Tuesday, December 12, 11-12pm ET — Register December 12, 2023.
- Monday, December 18, 4-5pm — Register December 18, 2023.
Not registered for Availity yet?If you aren’t registered to use Availity Essentials, signing up is easy and 100% secure. There is no cost for your providers to register or to use any of our digital applications. Start by going to Availity.com and selecting New to Availity? Get Started at the top of the home screen to access the registration page.
If you have questions regarding registration, reach out to Availity Client Services at 800‑AVAILITY (800-282-4548). Start using Availity Essentials PDM today to improve your provider data management experience. Exclusions:- Behavioral health providers assigned to Carelon Behavioral Health, Inc. will continue to follow the process for demographic requests and/or roster submissions, as outlined by Carelon Behavioral Health.
- Any specific state mandates or requirements for provider demographic updates.
* If any roster data updates require credentialing, your submission will be routed appropriately for further action. Carelon Behavioral Health, Inc. is an independent company providing utilization management services on behalf of the health plan. COBCBS-CRCM-041492-23-CPN41168 When you have more information to share about a claim that has been denied, filing the dispute digitally is a cost-effective and time-saving alternative to paper and fax. You can feel confident that we have received your claims dispute when you submit it through the digital workflow. This Claim Status application feature, available on Availity.com, enables a fast, efficient, and streamlined process for filing claim disputes: - Upload supporting documentation and attach it directly to the claim.
- Use the Appeals Dashboard:
- To review digitally filed disputes.
- To retrieve correspondence related to your disputes.
- For a history of digitally filed disputes.
How to file a digital claim payment dispute:- Log onto Availity.com.
- Select the Claims & Payments tab.
- Select Claim Status and enter the information needed to retrieve your claim.
- When you have found your claim, select the Dispute button to initiate a dispute (it will be visible when your claim is eligible for a dispute).
- Access your Appeals Dashboard to upload the supporting documents, locate initiated dispute, and complete the dispute request:
- From the Claims & Payments tab select Appeals to access your Appeals Dashboard.
In the past, you may have used the Attachment button and selected the Dispute option to dispute a claim. We’ve eliminated that process to make disputing a claim more trackable and transparent. 
Receive dispute determinations digitally from your Appeals DashboardWe will review the dispute and communicate an outcome on Availity.com. Check the status of a digitally submitted dispute at any time from your Appeals Dashboard. Learn moreSubmitting a digital claim payment dispute is easy, but attending informative learning sessions provides a deep dive into the application and its search and filter functions. These tips are sure to make the submission process even easier. Use this link to access on-demand training. For more information about the claim payment dispute process, consult the provider manual or reach out to your provider relationship management representative. MULTI-BCBS-CM-041338-23-CPN41106 Anthem continues to work to enhance our provider data management system, which should significantly improve your data accuracy, transparency, and experience. In April 2023, we mailed letters notifying our care provider partners about our plans to begin implementing changes to our data management system. Since that time, we’ve included reminders in our provider newsletter, Provider News. We completed the implementation of these changes in September 2023. What is important? - As a reminder, you are contractually required to report any practice changes.
- Tell us when providers join your group. Notifying us in a timely manner prior to the new provider rendering care to our members is important.
- Ensure all your contracted providers’ information is uploaded into our provider data management system prior to rendering services.
- Claims received for services rendered by a provider who has not yet been added to your contract will be rejected or processed as out of network.
As we communicated in October, Availity Essentials Provider Data Management (PDM) is the intake application for care providers to submit demographic change requests, including submitting roster uploads. Availity Essentials PDM will replace all current intake channels for demographic change requests and roster submissions as of January 1, 2024. Read the previously published articles here: Providers should continue to use the Provider Enrollment application in Availity Essentials to submit requests to add new practitioners under existing groups. What you need to know about billing As part of this data management system upgrade, Anthem is applying CMS billing guidelines to hold care providers accountable for billing claims data correctly. Beginning in early 2024, claims submitted using rendering providers who have not been added to your contract by the date of service billed or with missing or incorrect NPIs will be rejected for more information or processed as out of network. Other important and helpful remindersSubmitting claims with complete and correct information is critical to ensuring Anthem can process your claims efficiently and accurately: - Bill according to standard billing guidelines.
- Review your billing practices carefully to ensure the proper TIN, NPI, and rendering provider information (if applicable) are submitted correctly.
More information is available online at anthem.com/provider > Providers > Policies, Guidelines & Manuals or at this link. CMS regulations and guidance can be found here. COBCBS-CRCM-041489-23-CPN40954 As part of our credentialing process, practitioners have certain rights as briefly outlined below. Practitioners can request to: - Review information submitted to support their credentialing application.
- Correct erroneous information regarding a credentialing application.
- Be notified of the status of credentialing or recredentialing applications.
We encourage practitioners to begin the credentialing process by going to availity.com as soon as possible when new physicians join a practice. Doing so will help minimize any disruptions to the practice and members’ claims. COBCBS-CM-035731-23-CPN33992 Effective for dates of service on and after November 5, 2023, the following updates will apply to the Carelon Medical Benefits Management, Inc. Clinical Appropriateness Guidelines for medical necessity review for Anthem Blue Cross and Blue Shield: - Musculoskeletal Guidelines:
Existing precertification requirements have not changed. Share this notice with other members of your practice and office staff. Through our efforts, we can help our care provider partners deliver high quality, equitable healthcare. Carelon Medical Benefits Management, Inc. is an independent company providing utilization management services on behalf of the health plan. MULTI-BCBS-CR-037766-23-CPN37065 THIS ARTICLE WAS PUBLISHED IN ERROR AND RETRACTED ON 11/30/23 ACCESS THE UPDATED ARTICLE FOR YOUR STATE BELOW: Colorado
Connecticut
Georgia
Indiana
Kentucky
Missouri
Ohio
Nevada
New Hampshire
Virginia
Wisconsin Effective February 1, 2024, prior authorization (PA) requirements will change for the following codes. The medical codes listed below will require PA by Anthem Blue Cross and Blue Shield for Medicare members. Federal and state law, as well as state contract language and Centers for Medicare & Medicaid Services guidelines, including definitions and specific contract provisions/exclusions take precedence over these precertification rules and must be considered first when determining coverage. Non-compliance with new requirements may result in denied claims.
Prior authorization requirements will be added for the following codes:
Codes
| Description
| 33274
| Transcatheter insertion or replacement of permanent leadless pacemaker, right ventricular, including imaging guidance (such as fluoroscopy, venous ultrasound, ventriculography, femoral venography) and device evaluation (such as interrogation or programming), when performed
| 33275
| Transcatheter removal of permanent leadless pacemaker, right ventricular
|
Not all PA requirements are listed here. Detailed PA requirements are available to providers on Medicare Advantage Providers | Anthem.com, select your state > Providers > Claims > Prior Authorization. For contracted providers, access Availity.com. Providers may also call number on the back of their patient’s member ID card for Provider Services.
UM AROW 4290 Anthem Blue Cross and Blue Shield is the trade name of Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc. Independent licensees of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CR-041041-23-CPN40476 Effective February 1, 2024, prior authorization (PA) requirements will change for the following code(s). The medical code(s) listed below will require PA by Anthem Blue Cross and Blue Shield for Medicare Advantage members. Federal and state law, as well as state contract language and Centers for Medicare & Medicaid Services guidelines (including definitions and specific contract provisions/exclusions), take precedence over these precertification rules and must be considered first when determining coverage. Non-compliance with new requirements may result in denied claims. Prior authorization requirements will be added for the following code(s): Code | Description | J1411 | Injection, etranacogene dezaparvovec-drlb, per therapeutic dose |
Not all PA requirements are listed here. Detailed PA requirements are available to providers on https://www.anthem.com/medicareprovider on the Resources tab or for contracted providers by accessing Availity.com.* Providers may also call Provider Services at the number on the back of the patient’s member ID card for assistance with PA requirements. * Availity, LLC is an independent company providing administrative support services on behalf of the health plan. MULTI-BCBS-CR-038834-23-CPN38083 Effective April 1, 2024, Carelon Medical Benefits Management, Inc. will expand multiple programs to perform medical necessity reviews for additional procedures for Anthem Blue Cross and Blue Shield members. Carelon Medical Benefits Management works to improve healthcare quality and manage costs for today’s most complex and prevalent tests and treatments, helping to promote care that is appropriate, safe, and affordable. The expansion will require clinical appropriateness review for additional procedures related to the Carelon Medical Benefits Management cardiology, genetic testing, radiology, musculoskeletal, surgical and radiation therapy programs. Carelon Medical Benefits Management will follow the clinical hierarchy established by Anthem Blue Cross and Blue Shield for medical necessity determination. Anthem Blue Cross and Blue Shield makes coverage determinations based on CMS guidance, including national coverage determinations (NCDs), local coverage determinations (LCDs), other coverage guidelines and instructions issued by CMS, and legislative changes in benefits. When existing guidance does not provide sufficient clinical detail, Carelon Medical Benefits Management will determine medical necessity using an objective, evidence-based process. Carelon Medical Benefits Management will continue to use criteria documented in Anthem Blue Cross and Blue Shield’s Medical Policies and Clinical Guidelines listed in the table below. These Clinical Guidelines can be found at Availity.com. Detailed prior authorization (PA) requirements are available online by accessing the Precertification Lookup Tool under Payer Spaces at Availity.com. Contracted and noncontracted care providers should call Provider Services at the phone number on the back of the member’s ID card for PA requirements. Prior authorization review requirementsCarelon Medical Benefits Management will begin accepting PA requests on March 18, 2024, for dates of service April 1, 2024 and after. For procedures scheduled to begin on or after April 1, 2024, care providers must contact Carelon Medical Benefits Management to obtain PA for the below non-emergency modalities. Refer to the Clinical Guidelines on the microsite resource pages for complete code lists. Program | Services | Medical Policies or Clinical Guidelines | Cardiology | •Cardiac monitor device •Cardiac contractility modulation | CG-MED-74 SURG.00153 | Genetic testing | •Chromosomal microarray analysis •Gene expression profiling •Gene mutation testing •Gene sequencing •DNA-based prenatal testing •Panel and other multi-gene testing for polymorphisms •Genetic testing for inherited diseases •Molecular marker evaluation of thyroid nodules •Hybrid personalized molecular residual disease testing for cancer | CG-GENE-04 CG-GENE-10 CG-GENE-13 CG-GENE-14 CG-GENE-21 CG-GENE-22 GENE.00010 GENE.00023 GENE.00052 GENE.00053 GENE.00056 GENE.00057 GENE.00059 TRANS.00025 | Radiology | •Radiostereormetric analysis •Breast MRI | Breast MRI guideline RAD.00065 | Musculoskeletal | •Percutaneous and endo spinal surgery •Open SI joint fusion •Ultrasound bone growth stimulation •Cryoablation for podiatric conditions •Nerve stimulation devices for pain | SURG.00071 SURG.00100 SURG.00147 SURG.00158 | Surgical | •Tx of GE reflux, dysphagia, gastroparesis | SURG.00047 | Radiation therapy | •Hyperthermia for cancer therapy | CG-MED-72 |
To determine if PA is needed for a member on or after April 1, 2024, call Provider Services using the phone number on the back of the member’s ID card. Care providers using the interactive care reviewer (ICR) tool on Availity.com for PA requests on an outpatient procedure will receive a message referring the provider to Carelon Medical Benefits Management. (Note: ICR cannot accept PA requests for services administered by Carelon Medical Benefits Management.) How to place a review requestCare providers may place a PA request online to Carelon Medical Benefits Management via providerportal.com. ProviderPortalSM is available 24/7, processing requests in real-time using clinical criteria. For more informationFor resources to help your practice get started with the radiology, cardiology, genetic testing, musculoskeletal, surgical, and radiation oncology programs, visit: Our website helps you access information and tools such as order entry checklists, Clinical Guidelines, and FAQs. Through genuine collaboration, we can simplify access to care and help you deliver high-quality, equitable healthcare. Carelon Medical Benefits Management, Inc. is an independent company providing utilization management services on behalf of the health plan. Availity Essentials is an independent company providing prior authorization and billing services on behalf of the health plan. MULTI-BCBS-CR-038666-23-CPN38554 Effective September 13, 2023, the Related Coding section of the Pharmaceutical Waste – Professional and Facility reimbursement policy was updated to include Modifier JZ (zero drug amount discarded or not administered to any patient) as a new informational modifier. As a reminder, the intent of this policy is to require providers to use the most cost-effective vial or combination of vials of pharmaceutical when procuring and preparing a dose for administration to avoid pharmaceutical wastage. This applies to any non-self-administered drug or biologic dosage prepared from a single-dose vial (SDV). For specific policy details, visit anthem.com/provider/policies/reimbursement/?cnslocale=en_US_co Visit the Drug Lists page on our provider website at https://www.anthem.com/ms/pharmacyinformation/home.html for more information about: - Copayment/coinsurance requirements and their applicable drug classes.
- Drug lists and changes.
- Prior authorization criteria.
- Procedures for generic substitution.
- Therapeutic interchange.
- Step therapy or other management methods subject to prescribing decisions.
- Any other requirements, restrictions, or limitations that apply to using certain drugs.
The commercial and exchange drug lists are posted to the website quarterly on the first day of the month in January, April, July, and October. To locate the exchange, select Formulary and Pharmacy Information, and scroll down to Select Drug Lists. This drug list is also reviewed and updated regularly as needed. Federal Employee Program pharmacy updates and other pharmacy related information may be accessed at www.fepblue.org > Pharmacy Benefits. MULTI-BCBS-CM-018448-23, MULTI-BCBS-CM-041071-23-CPN41054, MULTI-BCBS-CM-044369-23-CPN44369 Healthcare Effectiveness Data Information Set (HEDIS®) is a widely used set of performance measures developed and maintained by NCQA. These are used to drive improvement efforts surrounding best practices. HEDIS 2023 documentation for Childhood Immunization Status (CIS) Measure description: The percentage of children 2 years of age in the measurement year who had the following on or before their second birthday: - Four DTaP (diphtheria, tetanus, and acellular pertussis)
- Three IPV (polio)
- One MMR (measles, mumps, and rubella)
- Three HiB (haemophilus influenza type B)
- Three Hep B (hepatitis B)
- One VZV (chicken pox)
- Four PCV (pneumococcal conjugate)
- One Hep A (hepatitis A)
- Two or three RV (rotavirus)
- Two flu (influenza)
The measure calculates a rate for each vaccine and three combination rates. HEDIS 2023 documentation for Immunizations for Adolescents (IMA) Measure description: The percentage of adolescents 13 years of age in the measurement year who had the following: - One MenACWY (meningococcal)
- One Tdap (tetanus, diphtheria toxoids and acellular pertussis)
- Two or three HPV (human papillomavirus)
The measure calculates a rate for each vaccine and two combination rates. HEDIS measurement year 2023 documentation for Lead Screening in Children (LSC) Measure description: The percentage of children 2 years of age who had one or more capillary or venous lead blood test for lead poisoning by their second birthday. What we are looking for in provider medical records: - Immunization records from birth (Department of Health immunization records are acceptable).
- If available, newborn inpatient records documenting Hep B.
- For those immunizations not recorded on the immunization record, provide progress notes for: Immunizations administered, patient’s history of disease (chickenpox, Hep A, Hep B, measles, mumps, rubella).
- Anaphylaxis due to the Dtap, IPV, MMR, HIB, Hep B, VZV, PCV, Hep A, RV, or Influenza vaccines.
- Encephalitis due to the Dtap vaccine.
- Diagnosis of severe combined immunodeficiency, immunodeficiency, HIV, lymphoreticular cancer, multiple myeloma, leukemia, or intussusception.
- Meningococcal vaccine with a date of service on or between the member’s 11th and 13th birthdays.
- Tdap vaccine with a date of service on or between the member’s 10th and 13th birthdays.
- At least two HPV vaccines on or between the member’s ninth and 13th birthdays and with dates of service at least 146 days apart, or at least three HPV vaccines with different dates of service on or between the member’s ninth and 13th birthdays.
- Lead testing results and date (capillary or venous) on or before the child’s second birthday.
- Evidence of hospice services in 2023.
- Evidence patient expired in 2023.
Helpful hints:- Childhood immunizations and lead blood tests must be completed by the child’s second birthday.
- Assess immunization needs at every clinical encounter, including sick visits and when indicated, immunize.
- Ensure immunization records include all vaccines that were ever given, including hospitals, health departments, all former providers, include refusals, and contraindications.
- FluMist (LAIV) vaccination (only approved for ages 2 to 49) may be used for the second vaccination, however it must be given on the child’s second birthday to be compliant.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). MULTI-BCBS-CRCM-038697-23-CPN38591 The Controlling Blood Pressure (CBP) HEDIS® measure can be challenging. It not only requires proof of a blood pressure reading, but also that the patient’s blood pressure (BP) is adequately controlled. CBP care gaps can open and close throughout the year depending on if the patient’s most recent BP reading is greater than 138/89 mmHG. As we approach the end of the year, it is important that we have record of your patients’ BP readings and that you schedule any members who have not had a BP reading during 2023 or who have had high readings recorded this year. Tips when scheduling members to close CBP care gaps:- When scheduling appointments, have staff ask patients to avoid caffeine and nicotine for at least an hour before their scheduled appointment time.
- If possible, update your scheduling app or your reminder text message campaigns to include a reminder about abstaining from caffeine as well as a reminder to arrive early to avoid a sense of rushing.
Tips for lower BP readings during the appointment:- Ask the patient if they tend to get nervous at appointments and have higher readings as a result. If they do, take their BP at both the start and end of the appointment. Document the lower reading.
- Readings could vary arm to arm. If slightly elevated in one arm, try the other and document the lower reading.
Getting credit for adequately CBP readings:- Submit readings via Category II CPT® codes on claims:
Description | Code | Diastolic BP | CAT II: 3078F-3080F LOINC: 8462-4 | Diastolic 80 to 89 | CAT II: 3079F | Diastolic greater than/equal to 90 | CAT II: 3080F | Diastolic less than 80 | CAT II: 3078F | Systolic BP | CAT II: 3074F, 3075F, 3077F LOINC: 8480-6 | Systolic greater than/equal to 140 | CAT II: 3077F | Systolic less than 140 | CAT II: 3074F, 3075F |
- Ensure readings are carefully and appropriately documented within your electronic medical records (EMR) system.
- If you have questions on how to submit readings, speak to your care consultant or program manager.
- Be sure to adequately code patients who meet the exclusion criteria.
To learn more about our commitment to health equity visit My Diverse Patients. HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). Anthem Blue Cross and Blue Shield is the trade name of Rocky Mountain Hospital and Medical Service, Inc. HMO products underwritten by HMO Colorado, Inc. Independent licensees of the Blue Cross Blue Shield Association. Anthem is a registered trademark of Anthem Insurance Companies, Inc. MULTI-BCBS-CRCM-038111-23-CPN37873 Each year, the CDC encourages care providers and individuals to learn more about antibiotics by promoting antibiotic awareness in November. The CDC’s Be Antibiotics Aware educational effort encourages care providers to: - Prescribe antibiotics only when they are clinically indicated. Antibiotics are only needed to treat certain infections caused by bacteria, not viruses like those that cause COVID-19. Harm can be done by prescribing antibiotics that aren’t needed.
- Talk to patients about why they don’t need antibiotics for a viral respiratory infection, what to do to feel better, and when to seek care again if they don’t feel better.
- Write a prescription for symptom relief, such as rest, fluids, cool mist vaporizers, and over-the-counter medicine.
CDC’s Be Antibiotics Aware offers resources that help educate patients about antibiotic use at Antibiotic Use | CDC. This includes waiting/treatment room posters, pamphlets such as Antibiotics Aren’t Always the Answer, prescription pads for cold relief, and more. HEDIS® Measures that assess antibiotic prescribing The following HEDIS measures assess appropriate antibiotic dispensing for bronchitis/bronchiolitis, upper respiratory infection, and pharyngitis. These measures are used to identify, monitor, and improve antibiotic prescribing practices. Avoidance of Antibiotic Treatment for Acute Bronchitis/Bronchiolitis (AAB):This measure assesses the percentage of episodes for patients ages three months and older with a diagnosis of acute bronchitis/bronchiolitis that did not result in an antibiotic dispensing event. If prescribing an antibiotic to patients with acute bronchitis, be sure to use the diagnosis code for the bacterial infection and/or comorbid condition. Appropriate Treatment for Upper Respiratory Infection (URI):This measure calculates the percentage of episodes for patients three months of age and older with a diagnosis of upper respiratory infection that did not result in an antibiotic dispensing event. Reducing unnecessary use of antibiotics is the goal of this measure. Educate patients on the difference between bacterial and viral infections. Refer to the viral illnesses as a common cold, sore throat, or chest cold. Appropriate Testing for Pharyngitis (CWP):This measure reports the percentage of episodes for patients three years of age and older where the patient was diagnosed with pharyngitis, dispensed an antibiotic, and received a group A strep test. When patients present with symptoms of pharyngitis, ensure proper testing (for strep) is performed to avoid the unnecessary prescribing of antibiotics. Record the results of the strep test. For more information and coding guidelines, reference the HEDIS guides on the Anthem provider website. HEDIS is a registered trademark of the National Committee for Quality Assurance. MULTI-BCBS-CRCM-037929-23-CPN37569 Instead of submitting medical records for the HEDIS® hybrid project, use the Remote Electronic Medical Record (EMR) Access Service provided by Anthem. We offer providers the ability to grant access to your EMR system directly to pull the required documentation to aid your office in reaching compliance. Granting our team remote access to your EMR helps reduce the time and costs associated with medical record retrieval while improving efficiency and allowing your office to focus on patient care. We have a centralized EMR team experienced with multiple EMR systems and extensively trained annually on HIPAA, EMR systems, and HEDIS measure updates. We complete medical record retrieval based on minimum necessary guidelines: - We only access medical records of members pulled into the HEDIS sample using specific demographic data.
- We only retrieve the medical records that have claims evidence related to the HEDIS measures.
- We only access the least amount of information needed for a use, disclosure, or a request.
- We only save to file and do not physically print any PHI.
Getting started with Remote EMR Access is just one email away. Email Centralized_EMR_Team@anthem.com today. To learn more about our Remote EMR Access, view the frequently asked questions below. Q. How do you retrieve our medical records?A. We access your EMR using a secure website and retrieve only the necessary documentation by printing it to an electronic file we store internally, on our secure network drives. Q. Is this process secure?A. Yes, we only use secure internal resources to access your EMR systems. All retrieved records are stored on Anthem secure network drives. Q. Why does Athem need full access to the entire medical record?A. There are several reasons we need to look at the entire medical record of a member, including: - HEDIS measures can include up to a 10-year look back of a member’s information.
- Medical record data for HEDIS compliance may come from several different areas of the EMR system, including labs, radiology, surgeries, inpatient stays, outpatient visits, and case management.
- Compliant data may be documented or housed in a non-standard format, such as an in-office lab slip scanned into miscellaneous documents.
Q. What information do I need to submit to use your Remote EMR Access Service?A. Email Centralized_EMR_Team@anthem.com with the following information: Practice/facility demographic information (for example, address, National Provider ID, Taxpayer Identification Numbers, etc.) - EMR system information (for example, type of EMR system, required access forms, access type, etc.)
- List of current providers/locations or a website for accessing this list.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). MULTI-BCBS-CRCM-037995-23-CPN37863 HEDIS ® is a widely used set of performance measures developed and maintained by the NCQA. These are used to drive improvement efforts surrounding best practices. Measure descriptionThe percentage of discharges for members 18 years of age and older who had each of the following: - Notification of inpatient admission (can only be captured through medical record review)
- Receipt of discharge information (can only be captured through medical record review)
- Patient engagement
- Medication reconciliation post-discharge
What we are looking for in care provider records: - Notification of inpatient admission — documentation in the outpatient medical record must include evidence of receipt for notification of inpatient admission on the day of admission through two days after the admission (three total days) with evidence of the date when the documentation was received. Any of the following examples meet criteria:
- Communication about admission between inpatient care providers or ER and the member’s PCP or ongoing care provider (for example, phone call, e-mail, fax, information exchange, automated alert system, shared electronic medical record, or from the member’s health plan)
- Indication that the PCP or ongoing care provider admitted the member to the hospital
- Indication that a specialist admitted the member to the hospital and notified the member’s PCP or ongoing care provider
- Indication that the PCP or ongoing care provider placed orders for tests and treatments any time during the member’s inpatient stay
- Documentation that the PCP or ongoing care provider performed a preadmission exam or received communication about a planned inpatient admission. The time frame that the preadmission exam or planned inpatient admission must be communicated is not limited to the day of admission through two days after the admission (three total days)
- Receipt of discharge information — documentation in the outpatient medical record must include evidence of receipt of discharge information on the day of discharge through two days after the discharge (three total days) with evidence of the date when the documentation was received. Discharge information may be included in, but not limited to, a discharge summary or summary of care record, or in the structured fields in an electronic health record. At a minimum, the discharge information must include the following:
- The practitioner responsible for the member’s care during the inpatient stay
- Procedures or treatments provided
- Diagnoses at discharge
- Current medication list
- Testing results, or documentation of pending tests or no tests pending
- Instructions for patient care post-discharge
- Patient engagement — documentation in the outpatient medical record must include evidence of patient engagement within 30 days after discharge. Any of the following meet criteria:
- An outpatient visit, including office visits and home visits
- A telephone visit
- A synchronous telehealth visit where real-time interaction occurred between the member and care provider using audio and video communication
- An e-visit or virtual check-in (asynchronous telehealth where two-way interaction, which was not real-time, occurred between the member and care provider)
- Medication reconciliation — documentation in the outpatient medical record must include evidence of medication reconciliation and the date when it was performed. Medication reconciliation must be conducted by a prescribing practitioner, clinical pharmacist, physician assistant, or registered nurse. Any of the following meet criteria:
- Documentation of the current medications with a notation that the care provider reconciled the current and discharge medications
- Documentation of the current medications with a notation that references the discharge medications (for example, no changes in medications since discharge, same medication at discharge, discontinue all discharge medications)
- Documentation of the member’s current medications with a notation that the discharge medications were reviewed
- Documentation of a current medication list, a discharge medication list and notation that both lists were reviewed on the same date of service
- Documentation of the current medications with evidence that the member was seen for post-discharge hospital follow-up with evidence of medication reconciliation or review:
- Evidence that the member was seen for post-discharge follow-up requires documentation that indicates the care provider was aware of the member’s hospitalization or discharge
- Documentation in the discharge summary that the discharge medications were reconciled with the most recent medication list in the outpatient medical record. There must be evidence the discharge summary was filed in the outpatient chart on the date of discharge through 30 days after discharge (31 total days).
- Notation that no medications were prescribed or ordered upon discharge
- Exclusions:
- Evidence of hospice or palliative services in 2023
- Evidence patient expired in 2023
Helpful hints:- Documentation of a procedure/surgery that is typically performed inpatient (such as, aortic bypass) does not indicate that the care provider is aware of the hospitalization. Documentation of post-op/surgery follow-up alone does not indicate the care provider was aware of the hospitalization or discharge. Make sure documentation references the hospitalization, admission, or inpatient stay.
- If performing a pre-admission exam, document that it is a pre-admission exam.
- If performing a pre-surgical, pre-operative, or surgical clearance exam, the date of the admission must be documented.
- Implement process to receive automated alerts when a member is admitted or discharged from an inpatient facility.
- Review discharge medications with the member.
- Schedule post-hospital discharge following appointments and have the office call the member to remind them.
- Document a received date for discharge summaries and notification of inpatient admissions.
- Use the appropriate billing codes for Medication Reconciliation and Patient Engagement.
HEDIS® is a registered trademark of the National Committee for Quality Assurance (NCQA). MULTI-BCBS-CRCM-038738-23-CPN38596 You may have patients who cannot tolerate moderate or high-dose statin therapy but appear in your HEDIS® denominator for Statin Use in Persons With Cardiovascular Disease (SPC). By properly submitting the required exclusion criteria for this measure, you can improve your quality scores before the end of the year. The Statin Therapy Exclusion Guide is a great resource to learn more on what qualifies as an exclusion and how to submit the proper criteria. Tips for implementing best practices and improving your quality scores before the end of the year:- Properly code and submit exclusion criteria for members who cannot tolerate moderate or high-dose statin therapy. Reference the Statin Therapy Exclusion Guide.
- Educate members on the importance of adhering to their statin therapy regime and educate them on potential side effects. If they start to experience muscle pain or weakness, have them contact you to discuss their options.
- Statin therapy should be accompanied by lifestyle modifications, such as a healthy diet and exercise. Work with your patients to proactively identify and overcome any barriers that may prevent lifestyle modifications:
- If they cannot make it to the gym, talk with them about exercising at home.
- Encourage a healthy diet based on the patient’s culture and local availability:
- Reference this conversation guide for more information on how to discuss lifestyle modifications if your patient is of a different culture than your own.
- For those patients who can tolerate moderate or high-dose statin therapy, encourage them to do 90-day prescriptions or mail order to eliminate barriers that may prevent them from getting their prescription on-time. As the SPC measure is reliant on pharmacy claims to close the care gap, try to prescribe the lowest cost medication that will work for them to eliminate any undue financial burdens on the patient and discourage the use of pharmacy discount cards.
Patient care opportunitiesYou can find patient care opportunities within the Patient360 application located on Availity Essentials* Payer Spaces. To access the Patient360 application, you must have the Patient360 role assignment. From Availity’s home page, select Payer Spaces, then choose the health plan from the menu. Select the Patient360 tile from the Payer Space Applications menu and complete the required information on the screen. Gaps in care are located in the Active Alerts section of the Member Summary. * Availity, LLC is an independent company providing administrative support services on behalf of the health plan. MULTI-BCBS-CR-037897-23-CPN37097 |